-
PDF
- Split View
-
Views
-
Cite
Cite
Ayaka Nakashima, Ai Miyoshi, Takashi Miyatake, Ogita Kazuhide, Yokoi Takeshi, Perimenopausal invasive hyadatidiform mole treated by total abdominal hysterectomy followed by chemotherapy, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw142, https://doi.org/10.1093/jscr/rjw142
Close - Share Icon Share
Abstract
Gestational trophoblastic neoplasias (GTNs) are rare tumors that constitute <1% of all gynecological malignancies. GTNs in postmenopausal women are rare and usually malignant. We present a rare case of an invasive mole of the uterus with metastasis to the right ovary and labium minus treated by total abdominal hysterectomy followed by chemotherapy.
Introduction
Gestational trophoblastic neoplasias (GTNs) are rare malignant tumors arising from placental trophoblastic tissues. Approximately 50% of GTNs occur after molar pregnancies, 25% after normal pregnancies and 25% after ectopic pregnancies or abortions [1]. They are classified into four groups, namely, invasive mole, choriocarcinoma, placental site trophoblastic tumor and epithelioid trophoblastic tumor. Approximately 15–20% of complete hydatidiform moles and 1% of partial moles develop into one of the GTNs [2]. GTNs generally occur in reproductive age and are extremely rare in perimenopausal women. Invasive moles are responsible in most cases of localized GTNs. Invasive moles are characterized by extensive tissue invasion with trophoblasts and whole chorionic villi. Penetrating deep into the myometrium, sometimes with involvement of the peritoneum, adjacent parametrium or vaginal vault.
In the past, hysterectomy was a standard treatment for women diagnosed with GTNs of poor prognosis. However, this has changed since the introduction of highly effective chemotherapy, and GTN has become a disease that can be treated with chemotherapy alone in most cases. Although the role of hysterectomy has become limited in the modern treatment of GTN, the procedure may be necessary in certain cases [3].
Case Report
A 50-year-old woman, Gravida 3, Para 1, presented to our department with irregular genital bleeding for 2 months. Her last menstrual period had been 2 months before. Her obstetrical history included a normal vaginal delivery 13 years before and two spontaneous abortions 8 and 11 years previously. Transvaginal ultrasonography showed an enlarged uterus with endometrial thickening with an echogenic pattern (Fig. 1). As endometrial cancer was suspected first, an endometrial biopsy and magnetic resonance imaging (MRI) were performed. The endometrial biopsy revealed decidual tissues, and the MRI revealed invasion of a uterine corpus tumor into the myometrium (Fig. 2). A week later, the patient admitted to the hospital with continuation of irregular vaginal bleeding. Second endometrial biopsy was done and serum β-human chorionic gonadotropin (hCG) level was also measured owing to suspicion of a hydatidiform mole. The serum hCG level was over 225 000 mIU/mL, and the endometrial biopsy revealed a complete hydatidiform mole. Because the patient's hemoglobin level was 7.0 g/dL, owing to the continuation of uterine bleeding, we transfused 800 mL of red cell concentrate and discharged the patient. A lung metastasis, 1 cm in diameter, was observed on a contrast computer tomography scan (Fig. 3), and an invasive mole with lung metastasis was diagnosed. Because the patient did not desire preservation of her uterus or adnexa, we offered her a total abdominal hysterectomy (TAH) and bilateral salpingo-oophorectomy (BSO). At her next consultation for the continuous genital bleeding, a tumor of the right labium minus was recognized and histologically confirmed as a metastatic lesion of the mole (Fig. 4). The patient underwent TAH and BSO. Unfortunately, a tumor of right labium minus had spontaneously fallen off during surgery. In a gross specimen, molar vesicles were recognized at the uterine corpus with the right ovary a little swollen (Fig. 5). The invasions into myometrium by both villi and the trophoblasts were histopathologically confirmed (Fig. 6). In addition to the labium minus tumor, a metastatic lesion of the right ovary was diagnosed. The final pathological diagnosis was metastatic invasive hydatidiform mole, Stage III. The patient's serum hCG level fell to 10 779 mIU/mL after her operation. The patient was then started on administered methotrexate 20 mg/body intramuscularly, 5 days a week at 2 weeks intervals. Serum hCG levels are measured for the estimation of chemotherapy [4]. Her serum hCG level rapidly fell to 1.2 mIU/mL after four courses of methotrexate (Fig. 7). Two additional courses of methotrexate were completed, and there has been no evidence of recurrent disease for 6 months.

Transvaginal ultrasonography showing a endometrial thickening with echogenic pattern.
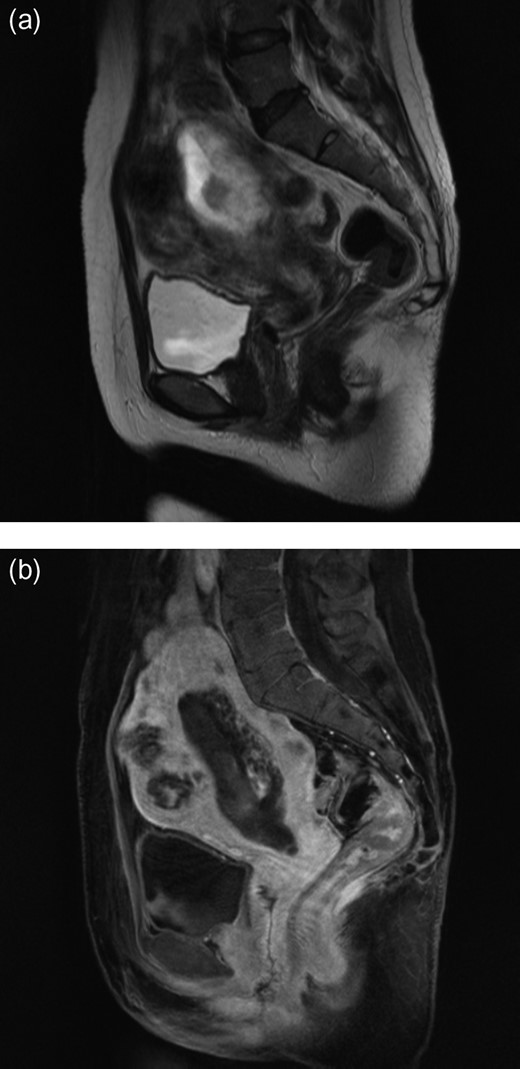
MRI showing invasion into the uterine cervix (a) and myometrium invasion in the posterior wall of the uterus (b).
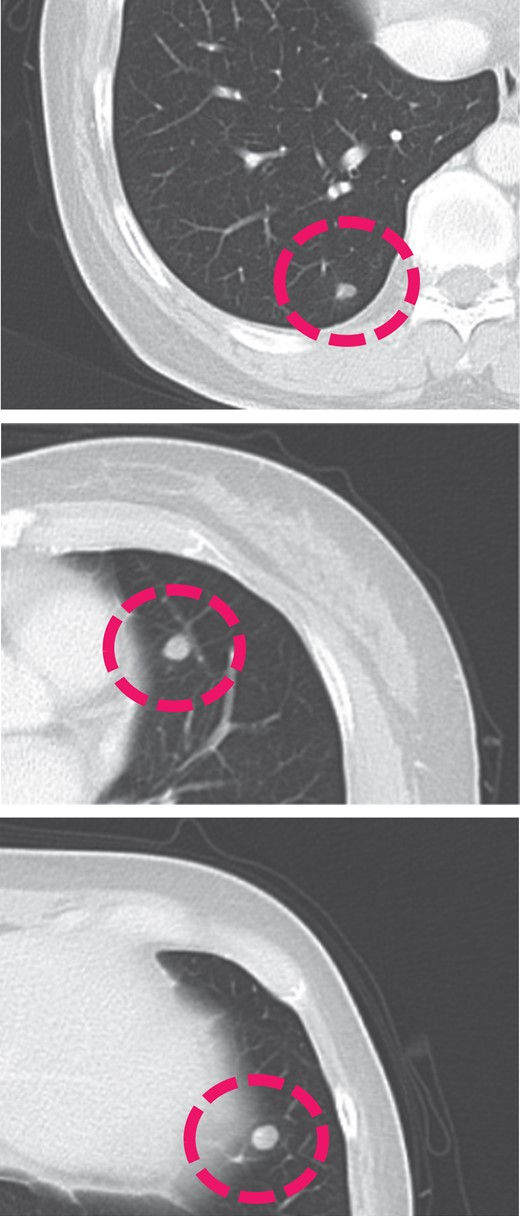
Contrast computed tomography scan showing the metastasis in the lungs.

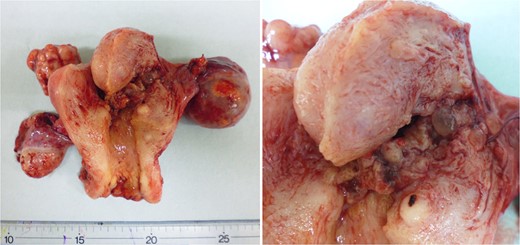
Gross specimen obtained after the TAH and bilateral salpingo-oophorectomy. In the close-up on the right, molar vesicles can be seen at the uterine corpus.
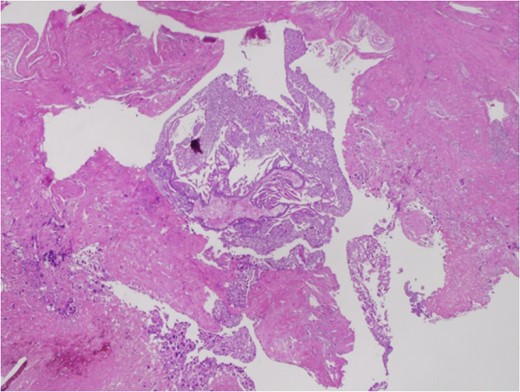
Histopathological staining shows the invasions into the myometrium by both the villi and trophoblasts.
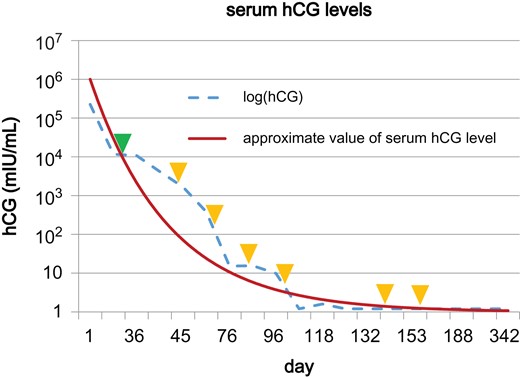
Graph showing the change in serum hCG levels from the first consultation to the end of treatment. The green triangle indicates when the patient underwent surgery (TAH and BSO), and the yellow triangle indicates methotrexate treatments.
Discussion
GTNs in postmenopausal women are rare and although, they can be benign or malignant in the perimenopausal and postmenopausal age group, they are usually malignant in the postmenopausal age group [5]. Over 20 years ago, Tsukamoto et al. reported 20 cases of trophoblastic disease in women aged 50 or older with 25% of the patients diagnosed with a choriocarcinoma, 35% with a hydatidiform mole and 40% with an invasive mole. However, none of the patients with hydatidiform mole were post menopausal [6].
The majority of women with GTNs are of reproductive ages and desire to preserve their fertility. Most GTNs can be treated with chemotherapy alone without hysterectomy [4]. In cases with metastatic GTN, a hysterectomy may be recommended for tumor reduction followed by chemotherapy. Indications for hysterectomy in the gestational trophoblastic disease cases, include women with no need to preserve fertility with a suspicious lesion confined to the uterus, a chemoresistant lesion, hemoperitoneum or coexistence of other uterine diseases [7]. Because GTNs are more likely to occur in older age groups—37.5% of patients are ≥50 years old versus 27.5% of patients 40–49 years old versus 13.9% of patients ≤15 years [8]—after molar evacuation, hysterectomy plays an essential role in the management of these patients. Hysterectomy decreases the overall risk for postmolar GTN to ~3.5% from 20% following suction dilation and evacuation [9]. Because most women with hydatidiform mole are of reproductive age <40 years old, the adnexa should not be removed unless the patient has an obvious adnexal metastasis, is perimenopausal or postmenopausal, or has complications related to theca lutein cysts [6]. Serum hCG levels must be monitored in all patients even after the hysterectomy to assure that no postmolar GTNs are arising.
Hysterectomy plays another important role in malignant GTN. Hammond et al. reported that when comparing similar patients at low-risk disease, patients undergoing primary hysterectomy followed by adjuvant chemotherapy had a shorter duration and lower total dose of chemotherapy than patients receiving chemotherapy alone [10]. Therefore, primary hysterectomy followed by chemotherapy is a reasonable solution for patients at low-risk GTN who do not desire to preserve fertility, especially for those of postmenopausal age.
When perimenopausal patients presented with irregular genital bleeding, we tend to think first of uterine cancer, but we must recognize gestational trophoblastic disease as one of the differential diagnosis.
Acknowledgements
Thank you very much to Ai Miyoshi for giving me a chance to make a case report. Also a big thanks to Takashi Miyatake for editing and advices for this paper.
Funding
There are no fundings.
Conflict of Interest statement
None declared.



