-
PDF
- Split View
-
Views
-
Cite
Cite
Kelly Lara, Esther Bae, Hanna Park, Farabi Hussain, A rare case of concurrent signet-ring carcinoma of breast and microangiopathic hemolytic anemia, Journal of Surgical Case Reports, Volume 2016, Issue 9, September 2016, rjw132, https://doi.org/10.1093/jscr/rjw132
Close - Share Icon Share
Abstract
Microangiopathic hemolytic anemia (MAHA) can be an uncommon presentation of an underlying malignancy, most often due to signet-ring cell carcinoma (SRCC). Additionally, pure SRCC in a breast primary-tumor comprises <2% of all breast cancers (Shin SY, Park H, Chae SW, Woo HY. Microangiopathic hemolytic anemia as the first manifestation of metastatic signet-ring cell carcinoma of unknown origin: a case report and review of literature. Kor J Lab Med 2011;31:157–61). To the best of our knowledge, the combination of these two entities, pure breast primary SRCC along with MAHA, has not been reported. Here, we present such a rare case. We also evaluate the current literature regarding this and similar disease processes, of which evidence is scarce and further research is needed.
Introduction
Microangiopathic hemolytic anemia (MAHA) has been demonstrated as the heralding sign of underlying solid tumor malignancy. It is often associated with signet-ring cell carcinoma (SRCC), which most commonly originates from gastric glandular cells, but may also originate from ovarian, lung and sometimes breast tissue [1]. SRCC of the breast is a rare entity, accounting for 2–4.5% of total breast carcinomas. Presentation as a pure SRCC in the breast is even more uncommon, with an unknown actual incidence [2]. To the best of our knowledge, there are no reported cases in which these two pathological rarities appear simultaneously. Here, we present such an account of a pure SRCC with breast primary, heralded by MAHA.
Case Presentation
A 34-year-old woman presented to an outside clinic with complaints of severe and progressive fatigue over a 3-week period. She had profound anemia and thrombocytopenia, and was immediately sent to our emergency department for further evaluation. Her initial studies revealed hemoglobin 3.3 g/dl, hematocrit 11.2%, platelets 23 000 cells/l and white blood cell count 17 000 cells/l. Her history and physical revealed no obvious source of her anemia. Additionally, she had bilateral breast densities that had been growing over the previous 3 weeks, nearly filling each breast to a diameter of 10 cm. The masses were mobile with no skin involvement or nipple retraction, with no fluid expressible from either nipple.
Evaluation of anemia and thrombocytopenia began with exploration of common causes. Mean corpuscular volume was 106 fl, red blood cell distribution width 30%. Manual blood count showed moderate polychromasia with both microcytic and macrocytic red blood cells. Schistocytes were visualized on blood smear. Haptoglobin was low (<15 mg/dl), while reticulocyte count was elevated (12.9%). Total iron and ferritin were both elevated (262 µg/dl and 1032 ng/dl, respectively). Vitamin B12 was elevated while folate was within normal limits. Initial imaging included computed tomography of her chest, abdomen and pelvis, which revealed diffuse skeletal metastases, masses in both breasts, hepatosplenomegaly and mesenteric stranding with trace ascites (Figs 1 and 2).

Computed tomography showing bilateral breast densities, showing nearly symmetric involvement of the entirety of each breast with no apparent chest wall or skin involvement.
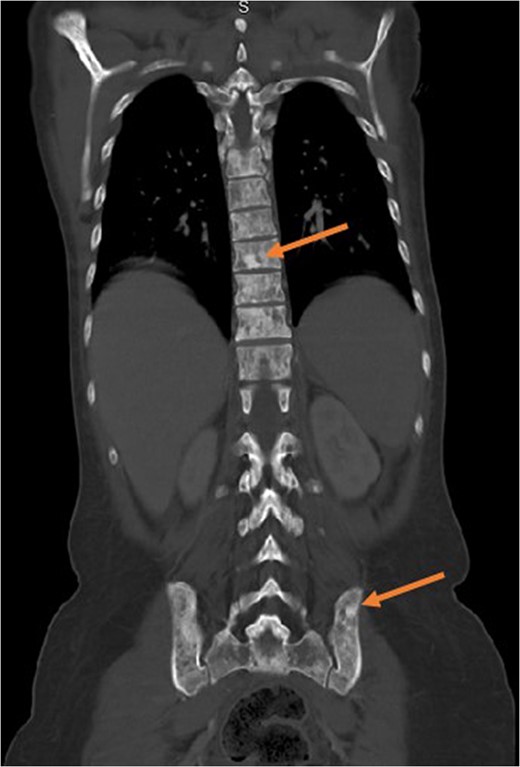
Computed tomography showing diffuse metastases to the spinal column and pelvis. This image exemplifies the propensity of signet-ring cells for bone and bone marrow, leaving other organs essentially untouched.
Core needle bone marrow biopsies demonstrated fibrotic and hypocellular (10% cellularity) bone marrow with infiltration of high grade, poorly differentiated metastatic carcinoma with some features suggesting breast origin and some features suggesting signet-ring cell origin. Core needle biopsies of both breasts identified high grade infiltrating signet-ring adenocarcinoma (Fig. 3A–C). The Her2/Neu assay was negative, while estrogen and progesterone receptors were strongly positive.
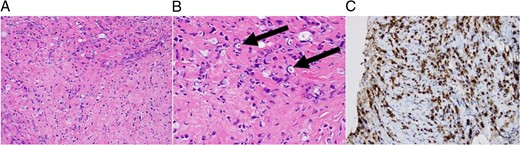
From left to right. (A) 200× magnification of CNB showing a field of fibrotic tissue with signet-ring cell. (B) 400× magnification highlighting signet-ring cells. (C) CA 15-3 antigen positivity on stain, suggestive of breast origin.
Discussion
The above laboratory values ruled out common vitamin and iron deficiencies as causes of her anemia. A microangiopathic origin is suggested by the schistocytes and low haptoglobin. Persistently low haptoglobin is often a sign of intravascular hemolysis and is related to conditions such as immune or hereditary thrombotic thrombocytopenic purpura (TTP) or cancer-associated MAHA (CA-MAHA) [3]. Both of these differential diagnoses could explain the thrombocytopenia. CA-MAHA can be often confused with TTP, but the best distinguishing factor is that CA-MAHA is Coomb's negative, whereas TTP is positive [4].
Shin et al. were able to identify 10 cases of SRCC which presented initially as MAHA [1]. Underlying cancer was identified of gastric origin in five patients. Ovarian and gastrointestinal origin accounted for one each, and the other three were of unidentified origin; none originated from the breast. Nine of 10 cases involved bone marrow and 5 of these were bony metastases. Time interval between the diagnosis and death was reported in seven cases, with mean life expectancy of ~2 months. This suggests that once MAHA is present, prognosis is poor. Ali et al. reported three cases in which MAHA was identified as a paraneoplastic syndrome of gastric SRCC; all three patients were deceased within 1 week of diagnosis. The authors note that each was diagnosed with a combination of peripheral blood smear and bone marrow biopsy, suggesting these to be keys factors in diagnosis [5].
Hemolysis in these patients is likely primarily due to fragmentation as it passes through small cancerous vessels. With the high rate of bone metastases, bone marrow involvement could be the mechanism by which hemolysis occurs in most patients, a mechanical hemolysis based on passage of the red blood cells through a fibrotic bone marrow bed [4]. Nearly all cases reported were either diagnosed with, or subsequently found to have, bone marrow involvement of the tumor burden. However, it has been observed that not all cases involved the marrow, and not all oncology patients with bone marrow metastases have CA-MAHA. This implies that the process is likely more complicated. Pendse et al. implicate high levels of von Willebrand factor (vWF) multimers and a functional deficiency of ADAMTS13/vWF-cleaving protease as contributors to the MAHA [6]. The exact mechanism remains unclear.
Although the prognosis is poor, there are treatment options, but these are almost entirely based on chemotherapy. Arkenau et al. reported two cases of MAHA as a paraneoplastic syndrome of metastatic SRCC. They claimed that in parallel to the symptomatic treatments of blood and platelet transfusions, chemotherapy was able to provide some control of the MAHA and slow the progression of malignancy [7]. Abdel Samie et al. reported on MAHA in a patient with SRCC of unknown primary. They conducted palliative chemotherapy with cisplatin, epirubicin and 5-fluorouracil continuous infusion. They observed an initial resolution of the anemia and regression of the bone metastases. However, the disease eventually progressed and the patient died 9 months later [8].
There is very little known about MAHA in patient with SRCC as a whole. There is almost no primary literature about the true incidence or treatment options for this disease process. Almost everything we know is based on sporadic cases reported over the years. Due to the rarity of paraneoplastic MAHA and the even more rare case of breast SRCC with MAHA, it is impractical to conduct any sort of prospective study. However, it could be beneficial to conduct a retrospective database analysis to identify a more accurate incidence of these cases, the incidence of involvement of each organ (breast, stomach, etc.), life expectancy, different treatment modalities and their effectiveness. A pilot study based on this brief report is indicated.
Conflict of Interest Statement
None declared.
Funding Sources
None.
References
Author notes
This a report of a patient presenting with an exceedingly rare case of microangiopathic hemolytic anemia due to metastatic signet-ring cell carcinoma of primary breast origin. This report highlights how little is known about this topic and similar entities, and that further investigation is warranted.



