-
PDF
- Split View
-
Views
-
Cite
Cite
M. Atie, O. Khoma, G. Dunn, G.L. Falk, Gastrointestinal tract obstruction secondary to post-operative oedema: does dexamethasone administration help?, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw139, https://doi.org/10.1093/jscr/rjw139
Close - Share Icon Share
Abstract
Oedema can occur in handled tissues following upper gastrointestinal surgery with anastomosis formation. Obstruction of the lumen may result in delayed return of enteric function. Intravenous steroid use may be beneficial. Three cases of delayed emptying following fundoplication, gastro-enteric and entero-enteric anastomoses are reviewed. Conservative management with supportive measures failed. Dexamethasone was administered to treat the oedematous obstruction. A literature review in PubMed, Cochrane database and Medline for English language publications on the use of dexamethasone in the treatment of acute post surgical oedema of the upper gastrointestinal was conducted. Administration of dexamethasone led to resolution of symptoms and successful outcome. No reports on the use of steroids in this context were identified in the literature. The use of dexamethasone may effectively treat intestinal obstruction due to inflammatory or oedematous cause in the early post-operative period.
Introduction
Temporary dysphagia is to be expected after anti-reflux surgery. This is normally self-limited and recovers over time [1]. Saliva regurgitation is an unwanted problem that is often associated with a tight fundoplication. Dilatation or revision surgery for continued severe dysphagia may be required [1]. Dysphagia may simply arise secondary to oedema in tissues following surgical manipulation. The use of dexamethasone, in selected cases, to reduce the oedema may help avoid an unnecessary endoscopic dilatation or reoperation. There are no reports in the surgical literature on this usage.
Similarly, oedema can occur in newly fashioned gastro-enteric and intestinal anastomoses [2, 3]. Early dysfunction of the conduit may occur as a result of either complete or partial obstruction by oedema. This is sometimes indistinguishable from an ileus without further investigation. Recognition of this scenario may enable timely management. The administration of steroids may reduce the peri-anastomotic oedema and allow early return of normal conduit function. Monitoring by computed tomography (CT) scanning has the potential of reduction in-hospital stay and parenteral nutrition. There are no reports in the literature on Dexamethasone usage in the latter scenario
Case Report
Three different clinical scenarios of oedema leading to conduit dysfunction in the early post-operative period are described. Conservative management had failed to relieve the relative obstruction. Administration of intravenous dexamethasone was beneficial.
Case 1
A 65-year-old female patient had undergone repair of a large hiatus hernia by laparoscopy with posterior cardiopexy and 360° fundoplication. Routine contrast swallow on Day 1 showed good passage of contrast through the fundoplication (Fig. 1a). On Day 2 post-operatively, saliva regurgitation occurred and repeat contrast study revealed a hold up at the level of the wrap (Fig. 1b). Intravenous dexamethasone (Merck Sharp & Dohme Laboratories-Chibret, France) administration at a dose of 8 mg daily was instituted for 72 h. Forty-eight hours later, oral fluid was tolerated allowing discharge and diet was upgraded to full fluids a week later. Recovery was progressive and uneventful with return to normal diet.
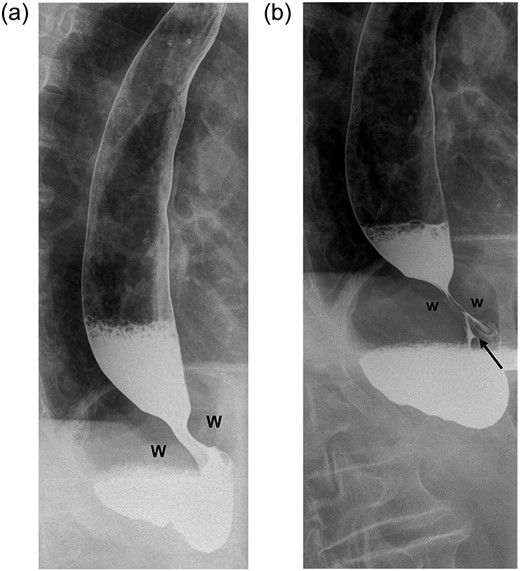
(a) Contrast swallow on Day 1 following posterior cardiopexy and 360° fundoplication demonstrating adequate passage of contrast through the wrap (W=right and left folds of the wrap). (b) A repeat contrast swallow in the same patient 24 h later revealing a hold up at the level of the wrap caused by oedema. The oesophagus above the wrap is dilated. A thin trickle of contrast (black arrow) is seen to come through the fundoplication.
Case 2
A 70-year-old Asian male underwent radical subtotal gastrectomy and D2 lymphadenectomy for TcisN0M0 gastric carcinoma. High naso-gastric output continued to Day 7. Contrast study showed hold up at the level of the anastomosis between the stomach and the Roux-en-Y gastro-jejunostomy (Fig. 2a). Intravenous dexamethasone at 8 mg daily was instituted for 72 h. Repeat contrast study showed good integrity of the anastomosis (Fig. 2b) and fluid diet was instituted. The patient was discharged 4 days after dexamethasone treatment and normal diet was established.
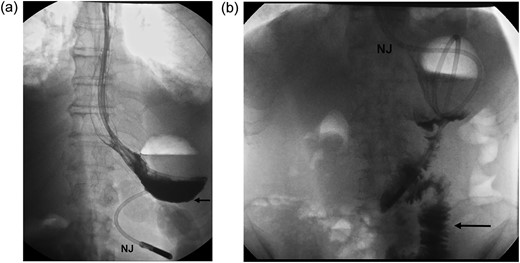
(a) An upper gastrointestinal series revealing hold up of contrast at the level of gastro-jejunostomy (black arrow), Day 7 post radical subtotal gastrectomy (b) A repeat contrast study, following dexamethasone challenge, shows good emptying with contrast reaching the jejunum (black arrow) promptly (NJ=naso-jejunal feeding tube).
Case 3
A 64-year-old Caucasian female underwent laparotomy for closed-loop small bowel obstruction secondary to adhesions from previous gynaecological surgery. Extensive division of adhesions was performed and small bowel resection was required for ischaemia. A side-to-side stapled entero-enterostomy was performed. Total parental nutrition was commenced due to a period of fasting prior to surgery and an expected protracted post-operative course. Prolonged ileus post-operatively, with abdominal distension and non-passage of flatus, continued to Day 9. CT scan showed non-passage of contrast at the anastomosis (Fig. 3a). Repeated enema and oral gastrograffin (Bayer, Germany) challenges failed. Dexamethasone 8 mg intravenously daily was instituted on Day 12 post-operatively. Bowel function returned spontaneously by Day 15 and repeat CT scan (Fig. 3b) with oral contrast showed complete resolution of the obstruction and proximal small bowel dilatation. Recovery occurred uneventfully.
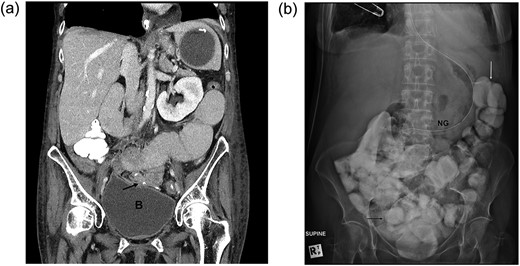
(a) CT scan of the abdomen and pelvis in a patient who underwent adhesiolysis and small bowel resection. The scan shows hold of the contrast at the level of the anastomosis (black arrow) just over the dome of the bladder (B=bladder). (b) A plain film of the abdomen, following Dexamethasone challenge, confirms the presence of contrast in the distal ileum (black arrow) and the colon (white arrow).
Discussion
There is extensive literature on the use of dexamethasone in the treatment of high-altitude cerebral and pulmonary oedema, neoplastic-related cerebral and spinal cord oedema, ophthalmic macular oedema and pharyngeal oedema [4, 5]. However, the literature on the use of steroids in the perioperative period is scant and mostly observational. There is a hesitancy amongst surgeons to use steroids immediately pre or post gastrointestinal surgery due to the potential inhibitory effects on healing and infection. There are no reports on the use of steroids to treat perioperative oedema of the gastrointestinal tract.
Wang et al. [6] examined the published literature between 1949 and 2011 for articles on the effects of corticosteroids on wound healing. The authors concluded that <10 days of high-dose corticosteroids had no important clinical effect on wound healing. Chronic corticosteroid treatment >30 days before surgery, increased wound-related complications by 2–5 times. The complication rates varied with dose and duration of steroid use, comorbidities and types of surgery.
Thornton et al. [7] report that healing in the gastrointestinal tract is rapid when free of complications. Risk factors are perioperative shock, hypoxia and resultant anastomotic ischaemia, irradiated tissues, sepsis and preoperative bowel obstruction. Steroid administration, malnourishment, malignancy, diabetes and age also influence outcome in a negative manner to varying degrees.
A systematic review and meta-analysis of the effect of perioperative steroids on ischaemia-reperfusion injury and surgical stress response in patients undergoing liver resection, found that patients receiving intravenous glucocorticoids were 24% less likely to suffer post-operative morbidity compared with controls [8].
In a meta-analysis of 15 observational studies evaluating 3807 patients undergoing 4189 operations for Crohn's disease, there was some evidence [OR: 1.99; 95% CI: 1.54–2.57] that steroid use may be associated with higher rates of intra-abdominal septic complications [9]. A study by Tzivanakis et al. [10] concluded that steroid usage and preoperative abscess were associated with higher rates of anastomotic complications following ileo-colic resection for Cohn's disease. In the absence of both steroids and intra-abdominal abscess, the risk of anastomotic complications was 6% but increased to 14% if either risk factor was present, and if both were present, the complication rate was 40%.
In summary, the results of steroid usage appear mixed in gastrointestinal surgery. There is low-grade evidence that short-term steroid usage is not disadvantageous. The three case experiences reported on the use of dexamethasone in a highly select group, where oedema was the suspect cause of delayed intestinal transit, were encouraging. Contrast studies or CT scanning have the potential to select patients with apparent obstruction secondary to intestinal oedema, isolate the site of hold up and exclude alternative causes. The index of suspicion for a mechanical problem was particularly low in our series of reports. The use of the steroids was short term and balanced against the risk of reoperation, parental nutrition and prolonged hospitalization. Rapid infusion of dexamethasone by a single shot is to be avoided in the conscious patient due to the incidence of severe perineal discomfort [11]. Slow infusion over 1 h is recommended.
In conclusion, intravenous steroids for treatment of oedematous dysfunction of intestinal conduits may be beneficial in the perioperative period in select cases. If further experience is positive, a randomized controlled trial may be justified.
Conflict of Interest Statement
None declared.
Disclosure
All of the authors have participated in caring for the patient, preparing and designing the intervention under review, acquiring the data, analysing and interpreting the data, draughting the article, revising it critically for important intellectual content and approving the final version to be submitted.
External Funding
None.
Previous Presentations or Publications
None.



