-
PDF
- Split View
-
Views
-
Cite
Cite
Masoomeh Khajehnoori, Sonal Nagra, Acute colonic pseudo-obstruction (Ogilvie's syndrome) with caecal perforation after caesarean section, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw140, https://doi.org/10.1093/jscr/rjw140
Close - Share Icon Share
Abstract
Ogilvie syndrome or acute colonic pseudo-obstruction is characterized by acute dilatation of the colon usually involving caecum and right hemi-colon in the absence of any mechanical obstruction. It is usually associated with an underlying severe illness/infection or surgery, mostly caesarean section and rarely occurs spontaneously. Identification of this condition is important due to the increased risk of bowel ischaemia and perforation particularly with caecal diameter >9 cm. This is a case report of bowel perforation following caesarean section leading to urgent laparotomy.
Case Report
A 40-year-old female G2P1 underwent an elective caesarean section at 38 weeks. Her medical history included thyroid carcinoma (papillary thyroid carcinoma) treated with thyroidectomy, bipolar affective disorder, mild obstructive sleep apnoea and a previous caesarean section.
On Day 1 post surgery she was noted to be tachycardic, febrile and hypertensive with a drop in saturation 92–93% on room air along with abdominal pain. Her differential diagnosis included atelactesis, pulmonary embolism and endometriosis (Fig. 1). On examination she had good bowel sounds, was passing flatus but had not opened her bowels. On Day 2 she had localized right lower quadrant tenderness with raised inflammatory markers of CRP 163, WCC 21 × 109/l and neutrophil count 17 × 109/l. The computed tomography (CT) scan of her abdomen/pelvis (A/P) showed evidence of ileus with dilated loops of bowel (Fig. 2).
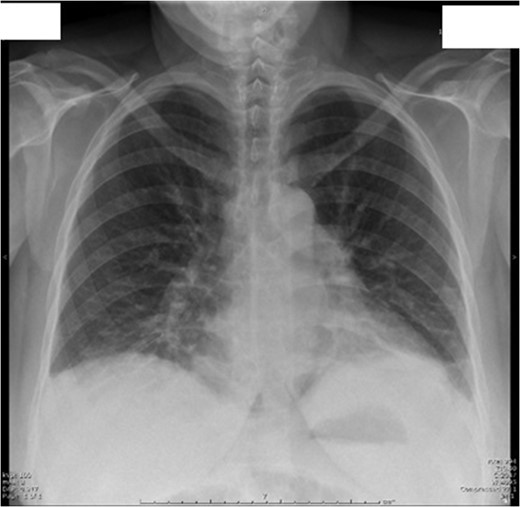
Day 1 postoperative chest X-ray shows evidence of mild atelactesis.
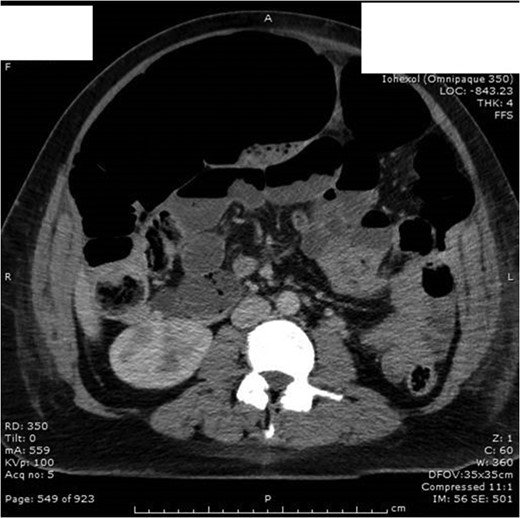
Day 2 post op CT A/P with no evidence of intra-abdominal collection/foreign body. Dilatation of entire intestine (large bowel up to 9 cm) most likely representing postsurgical ileus rather than a mechanical obstruction.
The next day she had fever with rigors, night sweats, ongoing abdominal pain and distension. Her bowel sounds were reduced and she had stopped passing flatus. She was treated for sepsis with likely respiratory source and commenced on intravenous antibiotics. On Day 4 post op she woke up with severe right shoulder tip and right upper quadrant pain radiating to her back. Her chest X-ray showed evidence of pneumoperitoneum (Fig. 3).
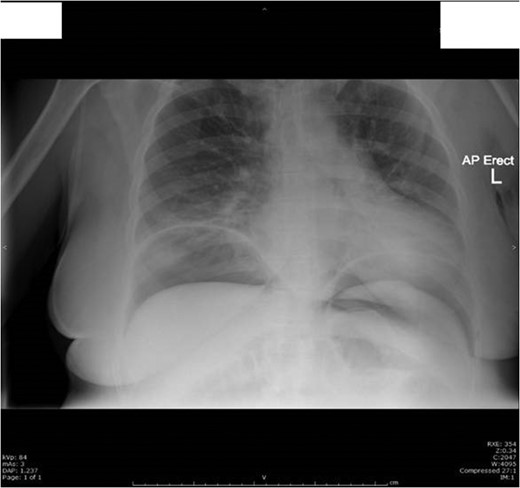
Day 4 post op chest X-ray showed a large volume of free gas under both hemi-diaphragms with multiple abnormally dilated loops of large and small bowel-features consistent with perforation of a hollow viscus.
She proceeded to have an emergency laparotomy with ileocolic resection and a double-barrel stoma. Operative findings were of perforation at base of caecum with mild faecal peritonitis and distended large bowel without evidence of malignancy or band adhesions (pseudo-obstruction complicated by caecal perforation).
Unfortunately post laparotomy she developed ileus (Fig. 4) and laparotomy wound dehiscence. Finally 13 days post laparotomy she was discharged home with district nursing for wound management and stoma care.

Day 3 post laparotomy she developed ileus with significant gaseous distension involving the large and small bowel; with multiple air-fluid levels on horizontal beam imaging.
Discussion
Ogilvie syndrome or acute colonic pseudo-obstruction is characterized by acute dilatation of the colon usually involving caecum and right hemi-colon in the absence of any mechanical obstruction [1, 2]. It is usually associated with an underlying severe illness/infection or surgery, mostly caesarean section and rarely occurs spontaneously [3]. The pathophysiology is unknown and is thought to be multifactorial. Disturbances of autonomic innervations of colon with imbalance in sympathetic and parasympathetic control of colon motility have been suggested as a potential contributing factor [1]. Compression of parasympathetic plexus by gravid uterus [4] and increased sympathetic stimulation due to stretch of mechanoreceptors within the wall of the colon causing decrease motility have been suggested [5]. Other theories like hormonal imbalance, hypoperfusion, metabolic and pharmacological causes have also been implied [6].
Diagnosis is made by clinical presentation of abdominal distension, constipation, nausea and vomiting. Bowel sounds have been noted to be present in 90% of patients [3]. Plain films show colonic distension mostly of caecum and ascending colon and CT scans help to exclude mechanical obstruction. Management is initially conservative with cessation of opioids, correction of electrolytes and active mobilization. Administration of neostigmine or colonoscopic decompression should be considered in patients with caecal diameter of >9 cm [2, 5]. Neostigmine is an anticholinesterase inhibitor and treatment targets ineffective colonic motility caused by either excessive sympathetic stimulation or parasympathetic dysfunction or both. It should be administered in ICU with continuous cardiac monitoring due to risk of bradycardia, with atropine readily available for urgent reversibility if required [7].
When the caecum is dilated >9 cm colonoscopic decompression is preferable as it reduces the risk of ischaemia and perforation. However, colonoscopic decompression has its own risks. It is not just a difficult procedure to perform in pseudo-obstruction; it also itself has an increased risk of perforation in Ogilvie's syndrome when compared to general population, as well as the risk of recurrence. Decompression in combination with neostigmine reduces the risk of recurrence [8]. Spontaneous perforation with increase in caecal diameter >9 cm has been reported in up to 15% of patients with a very high mortality rate [9]. If caecal diameter is >9 cm and findings are suggestive of bowel ischaemia, surgical intervention is urgently required [10].
Ogilvie syndrome if not treated can progress to bowel ischaemia and perforation with significant morbidity and mortality [2]. If detected early, conservative management is the first line of treatment with neostigmine or colonoscopic decompression. Failure of conservative management, caecal diameter of >9 cm and clinical suspicion of bowel ischaemia or perforation requires urgent surgical intervention.
Conflict of Interest Statement
None declared.



