-
PDF
- Split View
-
Views
-
Cite
Cite
Christel A.L. de Raaff, Wietse J. Eshuis, Bart A. van Wagensveld, Ruben N. van Veen, Complications of banded laparoscopic Roux-en-Y gastric bypass in a 33-week pregnant woman, Journal of Surgical Case Reports, Volume 2016, Issue 8, August 2016, rjw137, https://doi.org/10.1093/jscr/rjw137
Close - Share Icon Share
Abstract
Women desiring pregnancy might fail to conceive due to their obesity. Bariatric surgery has shown to reduce this infertility up to 58% and is therefore considered a successful strategy for morbidly obese infertile women. Nevertheless, when pregnancy has succeeded, surgery-related complications might occur.
Banded laparoscopic Roux-en-Y gastric bypass (B-LRYGB) is a relatively new technique in which a band is placed around the small gastric pouch. We report a case of a 30-year-old woman who succeeded to become pregnant after weight loss due to B-LRYGB, but presented with acute abdominal pain in Week 33 of her pregnancy.
Introduction
Obesity is associated with infertility and an increased risk of preterm birth in pregnant women [1]. Obese women desiring pregnancy are therefore advised to optimize their weight first. Women who are unable to achieve this weight loss with conservative therapies can decide to undergo bariatric surgery, which has shown to improve fertility up to 58% and to reduce adverse maternal and neonatal outcomes [2–4].
Bariatric surgery-related complications requiring acute abdominal surgery such as internal herniation after gastric bypass surgery might occur during pregnancy [5]. Additionally, cases of slippage of laparoscopic adjustable gastric banding (LAGB) are described in the literature [6].
Banded laparoscopic Roux-en-Y gastric bypass (B-LRYGB) is a relatively new technique and is believed to provide additional weight loss when compared with non-banded LRYGB [7]. However, no articles have been published regarding B-LRYGB-related complications during pregnancy.
We report a case of a 30-year-old woman who succeeded to become pregnant after weight loss due to B-LRYGB, but presented with acute abdominal pain in Week 33 of her pregnancy.
Case Report
A 30-year-old woman with a history of polycystic ovary syndrome (PCOS) visited the obesity center Amsterdam to opt for weight loss surgery. Due to her body mass index (BMI) of 41 kg/m2 and PCOS she had not succeeded to conceive. Patient underwent a LRYGB without any postoperative complications.
Four years later, she visited our hospital with complaints of weight regain and persistent irregular menstruation, and a still unfulfilled pregnancy wish. She claimed that her eating pattern had not changed, she was no sweetener and she exercised by cycling 40 km/week. A dynamic X-ray with barium contrast showed a dilated pouch. No abnormalities were found during esophagogastroduodenoscopy. During a multidisciplinary meeting, it was decided to revise the dilated pouch and apply a minimizer ring (Bariatric Solutions, Stein an Rhein, Switzerland) around the gastric pouch.
During surgery, the gastric pouch appeared not dilated, after which was decided not to revise the pouch and solely apply a minimizer ring (Bariatric Solutions, Stein an Rhein, Switzerland) 2 cm above the gastrojejunostomy. The minimizer ring was locked at the first hole (8 cm; diameter 2.55 cm) and fixated at the pouch with Vicryl (Ethicon Inc., a Johnson and Johnson Company, Somerville, NY, USA). No complications occurred in the 30-day postoperative period.
Patient became pregnant 6 months after B-LRYGB. Her excess weight loss was 28.1%; total BMI loss was 4.5 points and total body weight loss 14 kg. In the third week of pregnancy, patient visited our emergency room with epigastric pain with radiation to her back since 2 days. Vital parameters were normal, abdominal guarding was absent. Laboratory tests showed a C-reactive protein 36 mg/l, leucocytes 9.1 × 10 9/l and hemoglobin 6.1 mmol/l.
Computed tomography (CT) of the abdomen suggested dislocation of the minimizer ring possible internal intestinal herniation and dilation of the intestines (Fig. 1). No free air or fluid was identified. Contrast filled the gastric pouch and a small part of the alimentary limb. Further passage of contrast was not observed.
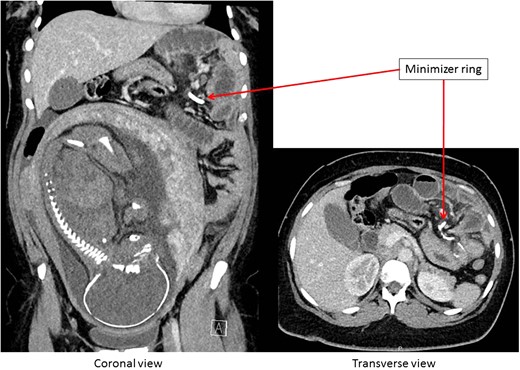
CT-scan of the abdomen showing an ileus caused by a migrated minimizer ring.
Therefore, patient received a nasogastric tube and was transferred to the operating room for emergency surgery. The fetus was monitored by a gynecologist with cardiotocography and the pediatrician was informed about the situation.
Diagnostic laparoscopy showed an ileus. Inspection along the alimentary limb resulted in locating the minimizer ring at the transition of alimentary limb and common channel. After removal of this ring, the biliopancreatic limb and common channel were visible again (Fig. 2). From the common channel, there were non-dilated intestinal limbs. The problem seemed resolved. There were no adverse outcomes for both the mother and the fetus.
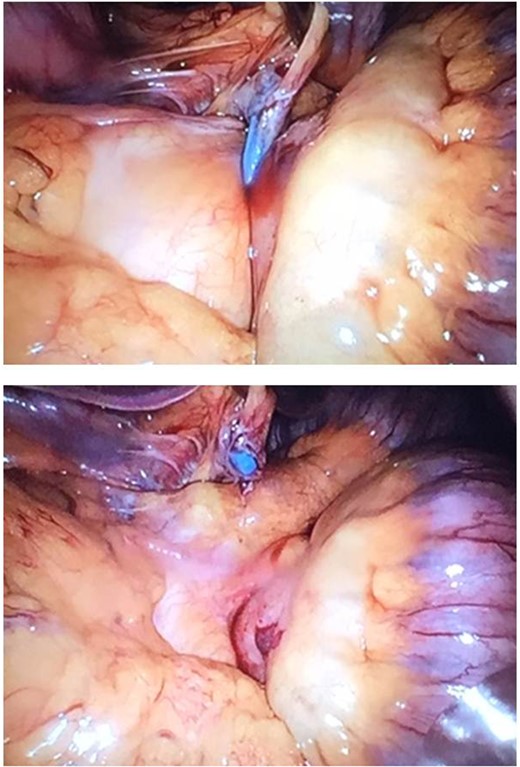
Upper picture: minimizer ring around the jejunojejunostomy. Lower picture: removal of the minimizer ring.
Since gastric retention was no longer present, the nasogastric tube was removed several hours post-surgery. Patient was discharged from the hospital the next day. No complications occurred. As patient desired a new minimizer, it was advised to discuss this when no further pregnancies were planned and only in case of weight regain.
Discussion
The prevalence of prepregnancy obesity continues to increase. In the USA, the prevalence was 17.6% in 2003, whereas this increased to 20.5% in 2009 [8].
A recent systematic review and meta-analysis reported improved pregnancy outcomes such as less preeclampsia and less gestational diabetes mellitus after bariatric surgery. However, there was an increased risk of small neonates and preterm birth. Although the authors conclude that more research is needed comparing pregnancy outcomes between several bariatric procedures, they recommend LAGB in women planning to become pregnant [9].
In the Netherlands, it is recommended to perform a laparoscopic sleeve gastrectomy in young women who want to become pregnant in future. This avoids the occurrence of gastric bypass-related complications such as internal herniation and band-related complications such as slippage.
However, when a young woman is scheduled for B-LRYGB, surgical precautions must be taken. During B-LRYGB surgery, the usage of insoluble suture material such as Mersilene instead of Vicryl should be considered in order to decrease the risk of band migration due to increased abdominal pressure during pregnancy.
In order to increase as much as perioperative safety as possible in pregnant women, several precautions could be taken: careful open introduction in the left upper quadrant, as high as possible, subcostal; usage of three trocars; left lateral lift to reduce vena cava pressure and increase venous backflow and perioperative cardiotocography.
Although the optimal time for pregnancy after bariatric surgery is unknown, it is recommended to delay pregnancy until the first postoperative year. A gynecologist should be involved during pregnancy.
Furthermore, women who remain overweight or obese due to insufficient weight loss following bariatric surgery are still at increased risk of adverse maternal and neonatal outcomes and should be regarded as a risk group [1, 10]. Extra follow-up during pregnancy is recommended.
Nevertheless, bariatric surgery has shown to be successful in the improvement of fertility and should be considered in morbidly obese women with a pregnancy wish, but fail to conceive due to their obesity.
Funding
None.
Acknowledgements
None.
Conflict of Interest Statement
None declared.



