-
PDF
- Split View
-
Views
-
Cite
Cite
Francesca Livi, Samuel Ndoro, John Caird, Darach Crimmins, Indirect cavernous carotid fistula in a 12-year-old girl, Journal of Surgical Case Reports, Volume 2016, Issue 6, June 2016, rjw095, https://doi.org/10.1093/jscr/rjw095
Close - Share Icon Share
Abstract
We present a very rare case of indirect cavernous carotid fistula (CCF) in a 12-year-old girl. Indirect CCF is extremely rare in the paediatric population. A 12-year-old girl presented with a 7-month history of frontal headaches and intermittent left-sided proptosis. On examination, she had dilated and engorged scleral veins on the left eye, mild dysdiadochokinesia and past pointing on the left side. A brain computer tomography with contrast, brain magnetic resonance imaging (MRI) and interventional radiography (IR) cerebral angiogram confirmed the diagnosis of CCF. The CCF was embolized and a follow-up brain MRI and an IR cerebral angiogram were conducted over the course of 8 months that revealed no evidence of residual CCF. CCF, though rare in the paediatric population, should be highly considered in the differential diagnosis when dilated scleral veins, proptosis and dysdiadokinesis are present in the clinical setting. Prompt treatment has good prognostic results.
Introduction
Spontaneous cavernous carotid fistula (CCFs) are less common than traumatic CCFs and are quite a rare entity in children. Their presentation widely varies, and diagnosis is commonly delayed due to late presentation to the hospital. Most CCFs are not life threatening; however, it is essential that CCFs be not overlooked in the paediatric population especially when dilated scleral veins, persistent headaches, proptosis and dysdiadochokinesis are present (Fig. 1).
Case report
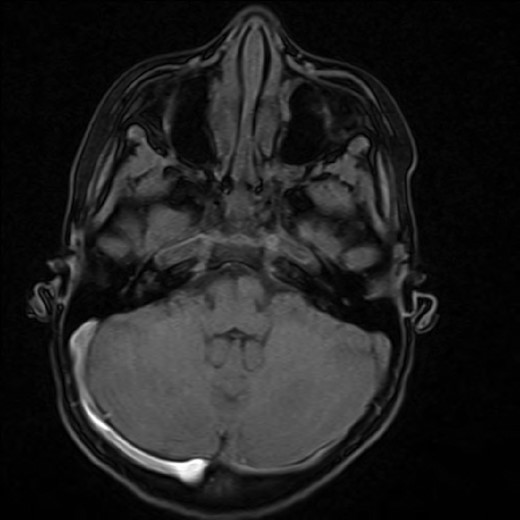
A 12-year-old girl presented with a 7-month history of frontal headaches and intermittent left-sided proptosis. On examination, she had dilated and engorged scleral veins on the left eye (evident on inspection), mild dysdiadochokinesia and past pointing on the left side. A brain computed tomography (CT) with contrast showed an enlarged left superior ophthalmic vein and a prominent left cavernous sinus. An interventional radiography (IR) cerebral angiogram under general anaesthesia was performed, which revealed evidence of an indirect CCF fed by ophthalmic branches of the left internal carotid artery and filling from multiple ethmodial branches of the distal internal maxillary artery. From the fistula, the ophthalmic vein was markedly hypertrophied and drained the cavernous sinus anteriorly. The fistula was also feeding from the right side through ethmodial branches into the right cavernous sinus and across to the left cavernous sinus (Fig. 2).
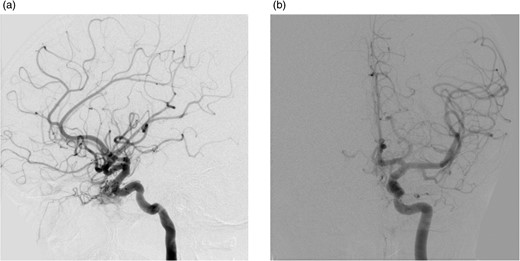
After a discussion that involved the neuroradiology team, neurosurgical team, the patient and her family, a decision was made to proceed with endovascular treatment of the fistula. Following informed consent from the patient's parents, the procedure was performed under general anaesthesia. Axis to the right common femoral artery was achieved with a 6-French micropuncture kit. A 6-French sheath was inserted into the right common femoral vein. A 6-French guide catheter was placed in the left internal jugular bulb. Thereafter, 4-French sheath was placed in the left common femoral vein. Then, a 4-French Weinberg catheter was placed in the left common carotid. A Headway microcatheter was advanced into the cavernous sinus trough the petrosal sinus into the cavernous sinus and subsequently into the dilated ophthalmic vein. Multiple coils were then placed into the ophthalmic vein throughout its course in the orbit back as far as the anterior section of the cavernous sinus. This resulted in near complete occlusion of the fistula. No immediate complications occurred, and the patient woke without any new neurological deficit in recovery (Fig. 3).
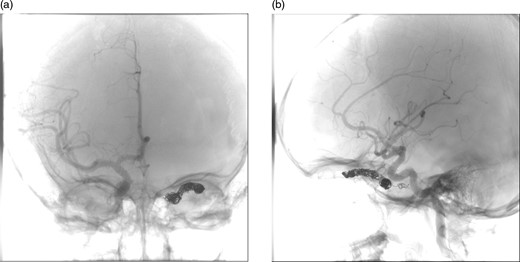
(a) and (b) Post-procedural digital subtraction angiogram under general anaesthesia shows no evidence of a residual CCF following coil embolization.
The patient was discharged 3 days later and a follow-up brain magnetic resonance imaging (MRI) was conducted 4 months afterward, which showed some residual proptosis. The superior ophthalmic vein was prominent but clearly less prominent than previous imaging. On a routine outpatient follow-up, her proptosis had significantly improved with reduction of the corneal injection, she reported no headaches and normal vision. A follow-up IR cerebral angiogram was conducted 4 months later that revealed no evidence of a residual CCF.
Discussion
A CCF is an abnormal communication between the internal or external carotid arteries and the cavernous sinus. These lesions may be classified based on aetiology (traumatic vs. spontaneous), velocity of blood flow (high vs. low) and anatomy (direct vs. dural, or internal carotid vs. external carotid) [1]. Barrow (1985) proposed a classification of CCFs into four subtypes based on their communication [2]. Type A CCF are direct high-flow shunts between the internal carotid artery and the cavernous sinus. Indirect fistulas are also referred to as dural cavernous sinus fistulas (DCSFs) because they are supplied by dural branches of both, external carotid artery (ECA) and internal carotid artery (ICA). Type B CCFs, DCSF, are dural shunts between meningeal branches of the internal carotid artery and the cavernous sinus. Type C CCFs, DCSF, are dural shunts between meningeal branches of the external carotid artery and cavernous sinus. Type D CCFs, DCSF, are dural shunts between meningeal branches of both the ICAs and ECAs and the cavernous sinus. Type D is the most frequent type often supplied by numerous branches from both territories, sometimes bilaterally. The Barrow classification does not, however, take into account cortical drainage nor does it differentiate between uniateral and bilateral supplies or fistulas [2–5].
Spontaneous CCFs are less common than traumatic CCFs and are a rare entity in children. They are usually found in postmenopausal women and patients with collagen vascular diseases and connective tissue diseases like Ehlers-Danlos syndrome and osteogenesis imperfecta. Iatrogenic causes include orbital floor fracture repair and cataract surgery. Ophthalmic manifestations range from proptosis, chemosis, orbital bruit, ptosis, vascular tortuosity, opthalmoplegia, glaucoma, chemosis, increased intraocular pressure and anterior segment ischaemia [1, 6–10]. In our case, the child presented with classic symptoms for a CCF; however, a delayed presentation ensured worsening complaints and symptoms. It is essential that CCFs be not overlooked in this clinical presentation even in the paediatric population.
Most CCFs are not life threatening; however, the involved eye is at considerable risk. Imaging studies, CT, MRI and IR cerebral angiography, may reveal an enlarged superior ophthalmic vein, thick ocular muscles and evidence of an enlarged cavernous sinus with convexity of the lateral wall. Treatment (surgical and endovascular) includes ligation of the external and/or internal carotid arteries and fistula embolization with glue, detachable ballons, microcoils and stents [10]. Microcoils were used in this case. Quick management with routine follow-up is essential for improved outcome as demonstrated in this case.
In conclusion, CCF is rare in the paediatric population; however, it is very important to keep a high degree of suspicion in the clinical setting of dilated scleral veins, proptosis and dysdiadokinesis. Prompt treatment has good prognostic results limiting the affected eye from considerable risk.



