-
PDF
- Split View
-
Views
-
Cite
Cite
Peter Werder, Renzo Bassetti, Johannes Kuttenberger, Surgical treatment option of the patent nasopalatine duct: a case report, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw090, https://doi.org/10.1093/jscr/rjw090
Close - Share Icon Share
Abstract
The nasopalatine duct (NPD) is a bilateral, epithelium-lined oronasal communication formed in the early fetal period. It connects the oral cavity with the nasal cavity within the primary palatal process. Mostly, the NPD obliterates during prenatal development and only epithelial remnants can be found after birth. A persistent NPD is therefore considered a developmental abnormality that often exists undetected without any clinical signs of discomfort. The presence of a persisting NPD, however, can be associated with pain sensation in the anterior maxilla. Differential diagnosis of the patent NPD is of importance, in order to prevent unnecessary therapy, such as endodontic treatment or tooth extractions. The present case report describes the diagnostic procedures, surgical treatment and follow-up of the patent NPD in a 53-year-old female patient suffering from maxillary pain caused by a patent NPD.
Introduction
In most mammals, the nasopalatine duct (NPD) exists as a viable, epithelium-lined oronasal communication. It connects the oral cavity with the nasal cavity, running from the incisive papilla to the nasal cavity [1]. In mammals, the NPD works as a transmission pathway for pheromones and chemosignals entering the oral cavity to the vomeronasal organ, also called ‘Jacobson’s organ’ [1].
In humans, the NPD is found as an intact canal only in the fetal period. During early prenatal development phases, the paired NPD runs within the same mesenchymal tissue as the nasopalatine nerve (NPN). In later development phases, a bony septum evolves on each side between the NPN and NPD, which separates them near the nasal cavity [2]. Thus, the incisive canal and the NPD must be considered two different anatomical structures [3]. The NPD almost always degenerates before birth and only epithelial remnants survive [4]. Only few case reports suggested the presence of a patent NPD in adults [3, 5–7].
The aim of this case report is to present a possible curative therapy in a patient suffering from maxillary pain caused by a patent NPD.
Case Report
A 53-year-old female patient was referred by her dentist with unclear pain in the anterior maxillary region after endodontic treatment and apical surgery at the teeth 12 and 11. Eighteen months before, the patient had suffered slight tooth trauma in the right maxillary front area (teeth 12 and 11).
Clinical examination revealed two small mucosal openings on either side of the incisive papilla, which could be probed partially (Fig. 1). Palpation of this area was painful. Two gutta-percha points were inserted into the two openings (Fig. 2). The cone beam computed tomography (CT) confirmed two patent NDPs with oronasal communication (Fig. 3).

Preoperative clinical situation: occlusal view of the maxillary arch presenting two small depressions of the mucosa on either side of the incisive papilla (blue arrows).

Occlusal view of the maxillary arch presenting two small openings of the mucosa with two inserted gutta-percha points on either side of the incisive papilla.
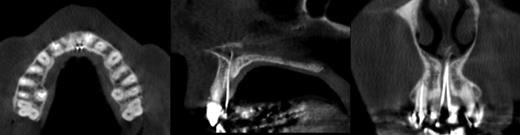
Gutta-percha points in the two NPDs showing communication between the oral and nasal cavities (cone beam CT: axial, sagittal and coronal sections).
Initially, a conservative treatment approach was performed. Both NPDs were rinsed with a 0.1% chlorhexidine solution (formula hospitalis; Hospital Pharmacy, Lucerne Cantonal Hospital, Switzerland) under local anesthesia (Ubistesin forte, 3 M, Rüschlikon, Switzerland), and Ledermix paste (Riemser, Greifswald, Germany) was applied into both openings. Three weeks after therapy, the symptoms had resolved and a non-irritated mucosal situation could be seen. Six months after the procedure, the patient was free of symptoms.
Few weeks after the 6-month follow-up, the symptoms came back and could not be resolved anymore by means of a conservative treatment approach. In accordance with the patient, a surgical approach was planned in order to achieve a ‘restitutio ad integrum’ (i.e. closure of the patent NPD).
According to the patient’s wish, the surgical treatment was carried out under general anesthesia. Local anesthesia (Ubistesin forte) as vasoconstrictive measure and premedication with amoxicillin/clavulanic acid (Co-Amoxi-Mepha, Mepha Pharma AG, Basel, Switzerland), starting 1 hour preoperatively (2 × 750/250 mg), were performed. Postoperative antibiotic medication was administrated for 5 days (3 × 500/125 mg/day).
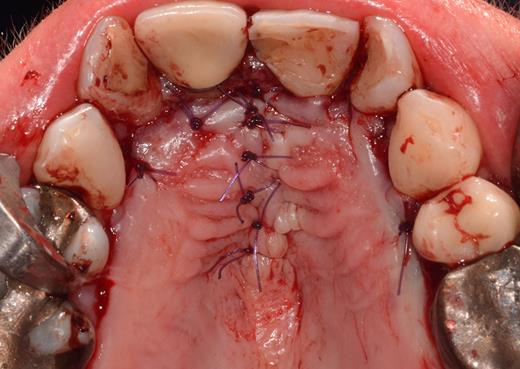
After a sulcular incision on the palatal side from teeth 15 to 25 and an incision in the midline of the palate omitting the incisive papilla and the two orifices of the NPD, two full-thickness mucoperiosteal flaps were raised. Thereafter, the incisive papilla and the whole contents of the incisive canal were enucleated (Figs 4–6). The bony incisive canal was filled with autologous bone harvested from the palatal region (bone scraper) (Fig. 7). A tension-free primary wound closure was achieved by moving the palatal flaps to the midline using single button and interdental vertical mattress sutures (Monocryl 4-0, Ethicon, Johnson & Johnson, USA) (Fig. 8). To avoid wound dehiscence and hematoma, an iodoforme gauze and a palatal plate were applied (Fig. 9). The patient was instructed to rinse three times a day with 0.1% chlorhexidine (formula hospitalis) for 2 weeks postoperatively. Sutures were removed after 14 days.
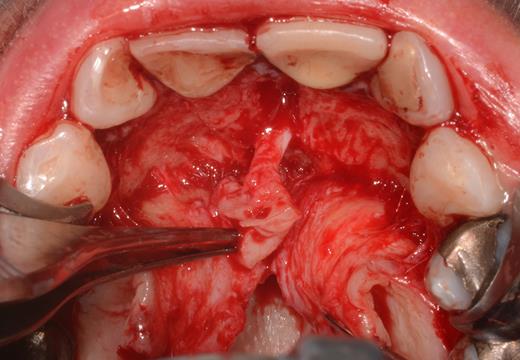
Preparation of the soft tissue of the incisive canal and the incisive papilla.

Situation after removal of the entire soft tissue contents of the incisive canal.

Excised soft tissue contents of the incisive canal including the neurovascular bundle and the incisive papilla.

Filling of the incisive canal using autologous bone harvested from the palatal region.

Coverage of the anterior palate with an iodoform gauze and a palatal plate.
Healing was uneventful and clinical examination confirmed the absence of the two small apertures. There were no signs of recurrence 6 months postoperatively (Fig. 10).

Site of initial manifestation of the patent NPD after 6 months with healthy mucosa and absence of orifices in the region of the anterior palatal mucosa.
Discussion
In this case report, the management of a symptomatical patent NPD in an adult is illustrated. A curative surgical treatment option in this context is suggested and documented.
A patent NPD may be identified, when it causes symptoms, or it may be diagnosed as an incidental finding. Due to the rare occurrence of pathologies in the incisive papilla area, many dentists may not pay particular attention to this region [5]. Moreover, the openings are mostly completely covered by the lateral portion of the incisive papilla [8]. Consequently, the anatomical variant of a patent NPD may easily be overlooked.
The following clinical symptoms may be indicative of a patent NPD:
debris collection, ability to produce squeaky noises,
persistent drainage, discharge [9],
passage of food/liquids into the nasal cavity [5],
bad taste in the mouth [9],
unclear pain/discomfort in the anterior maxilla, local swelling,
influx of air from the oral cavity into the nasal cavity,
soreness over the roof of the mouth [1],
discomfort in the anterior palatal region after complete denture mounting in the upper jaw, and
pain on mastication in the maxillary front area and a dull pain in the anterior hard palate region.
There are no standard treatment recommendations. Different procedures have been described, such as excision of the patent NPD after releasing a palatal full-thickness flap and subsequent coverage [1], chemical ablation [5] or conservative treatment options [7]. However, to date there has been no controlled clinical study investigating or comparing different treatment options for a symptomatic patent NPD. However, the therapeutic approach used is certainly not evidence based, but should give a possible guideline, when conservative treatment has failed. The surgical intervention presented in this case report aimed to achieve a ‘restitutio ad integrum’ by removing the entire soft tissue contents of the incisive canal and performing primary wound closure. Consequently, a possible residual sensory disturbance in the anterior palatal region between the canines has to be expected [10].
Considering the limitations of this case report, the surgical procedure presented above may be a possible therapeutic approach, if conservative treatment approaches have failed.
Conflict of Interest Statement
None declared.
References
Author notes
† Both authors contributed equally to the manuscript.



