-
PDF
- Split View
-
Views
-
Cite
Cite
Salman A.A. Jabbar, Nigel B. Jamieson, Andrew J. Morris, Karin A. Oien, Fraser Duthie, Colin J. McKay, Christopher R. Carter, Euan J. Dickson, A Glasgow Tipple—transjugular intrahepatic portosystemic shunt insertion prior to Whipple resection, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw089, https://doi.org/10.1093/jscr/rjw089
Close - Share Icon Share
Abstract
Abdominal surgery performed in patients with significant liver disease and portal hypertension is associated with high mortality rates, with even poorer outcomes associated with complex pancreaticobiliary operations. We report on a patient requiring portal decompression via transjugular intrahepatic portosystemic shunt (TIPS) prior to a pancreaticoduodenectomy. The 49-year-old patient presented with pain, jaundice and weight loss. At ERCP an edematous ampulla was biopsied, revealing high-grade dysplasia within a distal bile duct adenoma. Liver biopsy was performed to investigate portal hypertension, confirming congenital hepatic fibrosis (CHF). A TIPS was performed to enable a pancreaticoduodenectomy. Prophylactic TIPS can be performed for preoperative portal decompression for patients requiring pancreatic resection. A potentially curative resection was performed when abdominal surgery was initially thought impossible. Notably, CHF has been associated with the development of cholangiocarcinoma in only four previous instances, with this case being only the second reported distal bile duct cholangiocarcinoma.
Introduction
General surgery procedures in patients with significant liver disease, cirrhosis and concomitant portal hypertension are associated with high mortality rates [1]. Recently, minimally invasive transjugular intrahepatic portosystemic shunt (TIPS) procedures have replaced surgical portosystemic shunts. This technique is capable of reducing portal hypertension-associated complications leading to reduced intraoperative bleeding and perioperative complications in patients undergoing major extrahepatic surgery, but experience remains limited [1]. Pancreatic resection, in particular pancreaticoduodenectomy (PD) or Whipple resection, is associated with significant morbidity requiring detailed preoperative assessment and cautious patient selection in order to minimize complications [2]. The use of prophylactic TIPS for resectional cancer surgery is uncommon, with only a single report of utilization to achieve a major pancreatic resection [3]. Subsequently, we report on a patient undergoing portal decompression via TIPS prior to a Whipple resection, a combination referred to as the ‘Glasgow Tipple’.
Case Report
A 49-year-old male with no alcohol history presented to Glasgow Royal Infirmary with a 3-month history of right upper quadrant pain, jaundice, fever and 15 kg weight loss. Abdominal examination revealed hepatosplenomegaly, confirmed by abdominal ultrasound along with intrahepatic biliary tree dilatation. Liver function analysis revealed a mildly elevated bilirubin of 2.05 mg/dl. Computed tomography (CT) imaging demonstrated abrupt distal common bile duct (CBD) narrowing yet normal pancreatic duct. Notably, significant portal hypertension was evident with large para-esophageal varices and splenomegaly (Fig. 1a). With no obvious risk factors for chronic liver disease apart from obesity, alcoholic steatohepatitis was suspected. While magnetic resonance cholangiopancreatography was planned, cholangitis developed, prompting an ERCP, which revealed Grade B esophageal varices, an edematous ampulla (Fig. 1b) and a distal CBD filling defect, which was biopsied, with biliary drainage achieved using a plastic double pigtail stent. Histopathological examination revealed high-grade dysplasia within the bile duct adenoma. With potential for malignant progression, surgical resection was considered; however, comorbidity including obesity and sleep apnea compounded by portosystemic hypertension created a management dilemma.

(a) Preoperative CT scan revealed significant portal hypertension with large para-esophageal varices and splenomegaly. (b) ERCP image demonstrating the ampullary adenoma. (c) Liver biopsy reveals features in keeping with CHF.
Hepatic vein wedge pressure measured 30 mmHg compared to an arterial pressure of 12 mmHg confirmed portal hypertension; however, a fibroscan revealed no evidence of cirrhosis. Prophylactic β-blockers were commenced. Liver histology from a percutaneous biopsy suggested congenital hepatic fibrosis (CHF) as a potential underlying cause of portal hypertension (Fig. 1c). Following intense multidisciplinary discussion, it was decided that in the context of a relatively young, cardiovascularly fit patient with non-cirrhotic liver disease, a TIPS procedure was appropriate, with a view to reconsidering surgery. A literature search failed to identify evidence to support a decision to adopt a staged TIPS with PD for a high-grade dysplastic lesion.
Significant residual biliary dilatation remained, which prompted placement of a 6-cm partially covered metal wall stent with subsequent improved drainage. A Viatorr® stent graft (10 mm, Gore) was then placed between the middle hepatic vein and left portal vein. Pre-TIPS pressures measured as 19 mmHg was reduced to 7 mmHg postprocedure; unfortunately, this initial TIPS failed requiring a second, successful procedure (Fig. 2a).
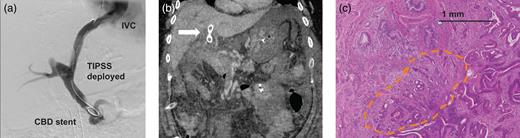
(a) Successful TIPPS deployment following insertion of a partially covered metallic biliary stent enabled portal decompression and resection to be performed. (b) Postoperative CT scan revealed failure of the TIPS (arrow) along with SMV thrombus resulting in significant venous congestion of the small bowel. (c) Histological examination of the resected specimen revealed a small cholangiocarcinoma.
Following further deliberation and no evidence of metastatic disease on imaging, the patient proceeded to resection. While fibroscan had suggested a normal liver, intraoperative fibrosis was encountered. Although few high-pressure veins were noted, the TIPS had achieved successful portal decompression enabling PD.
The patient subsequently developed postoperative pancreatitis, complicated on postoperative day 4 by respiratory distress requiring intensive care unit admission. CT imaging revealed small fluid collections related to the pancreatic anastomosis, which were not amenable to drainage. Strikingly, repeat CT scan on postoperative day 6 demonstrated TIPS failure with extension of thrombus into the superior mesenteric vein (SMV) and significant small bowel venous congestion. Despite the ominous appearance (Fig. 2b) conservative management with broad-spectrum antibiotics, inotropic support and low molecular weight heparin resulted in gradual improvement with discharge home achieved on day 28. Final pathology unexpectedly revealed a 15-mm pT1pN0 distal cholangiocarcinoma with clear resection margins (Fig. 2c), for which no adjuvant therapy was required.
Discussion
In the case presented above, portal hypertension potentially related to CHF was managed by preoperative TIPS insertion enabling curative PD for a cholangiocarcinoma. While the minimally invasive modality of a TIPS can reduce portal pressure in patients with severe liver cirrhosis, PD in patients with portal hypertension secondary to liver disease is traditionally contraindicated due to increased transfusion requirement and high mortality rate [4]. Previous studies have reported improved outcomes in patients undergoing TIPS placement prior to major nonhepatic surgery with a decrease in portal pressure improving surgical outcome due to reduced perioperative bleeding and ascites [5]. There were however no previous literature reports of this staged approach being utilized to facilitate a pancreatic resection. Once this strategy for mitigating risk had been chosen a resolute approach was followed. While complications following such a high-risk PD were not unexpected, postoperative TIPS failure with subsequent significant visceral venous congestion was not predicted and generated a challenging postoperative period for which a conservative strategy achieved a favorable outcome.
Of further interest is the diagnosis of CHF, a portobiliary system developmental disorder characterized histologically by defective ductal plate remodeling, progressive portal tract fibrosis and macroscopic cystic intrahepatic bile duct dilatation [6]. Clinical features include hepatomegaly, well-preserved hepatocellular function, portal hypertension resulting in splenomegaly, hypersplenism and gastro-esophageal varices [6, 7]. Furthermore, CHF is associated with ciliopathies (primary cilia disorders) that can result in renal disease [7]. Relative preservation of hepatocellular function despite hepatic fibrosis was a factor in the decision to undertake resection in the described case. There have been four reported cases of intrahepatic and a single extrahepatic cholangiocarcinoma occurring on the background of CHF, this patient being the second [6–9]. A potential mechanism by which the CHF intrahepatic biliary system undergoes malignant transformation may be the result of abnormal cholangiocyte cilia function [10].
This case demonstrates that in carefully selected patients with preserved liver function there may be a role for minimally invasive portal decompression to facilitate pancreatic resection for malignancy. While not without risk, our multidisciplinary strategy enabled a potentially curative resection for a patient for whom abdominal surgery would normally be contraindicated. We believe that carefully selected patients with pancreatic disease may benefit from this two-step approach and therefore assessment in further patient collectives are warranted.
Acknowledgements
The authors thank the staff members of the West of Scotland Pancreatic Unit and the surgical department.
Conflict of interest statement
None declared.
References
- edema
- liver diseases
- portal hypertension
- congestive heart failure
- weight reduction
- cholangiocarcinoma
- endoscopic retrograde cholangiopancreatography
- bile duct adenoma
- bile ducts
- jaundice
- pain
- pancreaticoduodenectomy
- transjugular intrahepatic portosystemic shunt
- preoperative care
- mortality
- liver biopsy
- hepatic fibrosis, congenital
- abdominal surgery
- pancreatic resection
- dysplasia



