-
PDF
- Split View
-
Views
-
Cite
Cite
Binod Bade Shrestha, Pradeep Ghimire, Dilasma Ghartimagar, Bishnu Jwarchan, Subita Lalchan, Mikesh Karmacharya, Mature brain tissue in the sacrococcygeal region, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw088, https://doi.org/10.1093/jscr/rjw088
Close - Share Icon Share
Abstract
Complete mature brain tissue in sacrococcygeal region is a rare congenital anomaly in a newborn, which usually is misdiagnosed for sacrococcygeal teratoma. Glial tumor-like ependymoma is also common in sacrococcygeal area but mostly appears later in life. We present a case of complete heterotopic brain tissue in the sacrococcygeal region. The patient underwent total excision of mass with coccygectomy. To our knowledge it is the second case being reported.
Introduction
Sacrococcygeal area is a common site for the rare developmental anomalies in a newborn, especially for germ cell tumors. Sacrococcygeal teratoma is one of the commonest diagnosis in this region and are benign 75% of the time, malignant and life-threatening 12% of the time. But we hereby report a very rare case of heterotopic brain tissue mimicking mature sacrococcygeal teratoma. So far only one case has been reported by Sugathadasa et al. [1].
Case Report
A term newborn baby girl had a swelling of the sacrococcygeal region. She had no other congenital anomalies and neurological deficit. Physical examination revealed a soft to solid oval mobile mass occupying the coccygeal, bilateral gluteal and intergluteal fold that measured 15 × 10 cm size. Skin surface showed slight bosselation of the surface without any ulceration. However, there was bluish to red discoloration of skin in posterior aspect of the mass (Fig. 1). On doing a rectal examination the mass could not be felt extending to the pelvis.

Gross swelling in sacrococcygeal region occupying bilateral buttock and intergluteal area.
Computed tomography (CT) and magnetic resonance imaging (MRI) of pelvis revealed a large mass of 14.5 × 9.5 cm in coccygeal, buttock and intergluteal fold without extension to adjacent structures. It showed a cystic to solid component with areas of hemorrhage. Unfortunately the CT and MRI films were lost on follow up. Echocardiography showed patent ductus arteriosus with small left to right shunt and mild pulmonary arterial hypertension with patent foramen ovale, which is supposed to be physiological. Serum markers like α-fetoprotein (AFP) and human chorionic gonadotropin (hCG) level were within normal limit. No preoperative tumor biopsy was done.
Total excision of tumor with coccygectomy was done under general anesthesia on the sixth day of life and the postoperative course was uneventful. Cut section surface showed nodular, solid gray white tissue with yellowish areas of fibrofatty tissue and small areas of hemorrhage (Fig. 2).

Cut section of the mass showing nodular, solid gray white tissue with yellowish areas and fibrofatty tissue.
Histologically, the section showed sheets of mainly brain tissue with mature glial cells and astrocytes (Fig. 3a). Gemistocytes with glial cells were seen showing abundant eosinophilic cytoplasm (Fig. 3b). Large areas showed sheets of oligodendrocytes with focal area of cystic spaces lined by cuboidal to columnar cells with papillary clusters of choroid plexus cells (Fig. 3c). There was no evidence of immature neuroepithelial component and yolk sac tumor component.
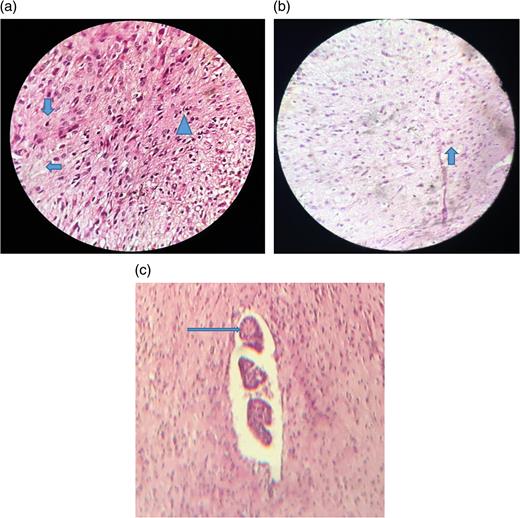
(a) Areas showing oligodendrocytes =  , astrocytes =
, astrocytes =  and fibrillary background =
and fibrillary background =  ; (b) Areas showing gemistocyte; (c) Picture showing choroid plexus with papillary projection lined by columnar epithelium.
; (b) Areas showing gemistocyte; (c) Picture showing choroid plexus with papillary projection lined by columnar epithelium.
Discussion
Newborn congenital anomalies, a birth defects are structural, functional, metabolic disorders and have a variety of etiology ranging from pregnancy or birth complications to genetic malformations to viral infections in utero. However, cause may be unknown in many cases. In a study by Malla [2] in a developing country like Nepal, the incidence of birth defects showed as 0. 36% among the total live births during one year at Maternity Hospital. Another study by Bhandari et al. [3] showed that the prevalence of congenital defects was 52.0 per 10 000 children while the prevalence of selected neural tube defects was 4.0 per 10 000 children.
Congenital malformation accounts for leading neonatal deaths and stillbirths, which is a result of poor antenatal care. In Nepal, in this study, the antenatal visits were made by 87.8% of women and only 63% of deliveries were carried out in hospital [4]. With musculoskeletal being the most common congenital anomalies in newborn, mass in sacrococcygeal may be benign or malignant.
Subcutaneous lipoma, neuroblastoma, myxopapillary ependymoma, neurofibroma, meningiomyelocele, sacrococcygeal teratoma, fetus in fetu, diastematomyelia, pilonidal sinus, sacral anomalies and perirectal abscesses are examples of mass in the sacrococcygeal region. Final diagnosis can be obtained by accurate history, general physical examination, radiological scanning, tumor markers like serum AFP and β-hCG level and finally with histological assessment.
Sacrococcygeal teratoma (SCT) that develops at the base of the coccyx, which is believed to be derived from primitive stalk, is the commonest tumor involving the sacrococcygeal region in newborn [5–7]. Benign SCTs are more likely to develop in younger children who are less than 5 months old. SCTs occur three to four times more often in girls than in boys [8]. Absence of tissue derived from all three germ layers and presence of only mature brain tissue excludes the diagnosis of SCT. Also absence of yolk sac element with normal value of AFP and hCG in these neonates further clarifies the diagnosis.
Diagnosis such as subcutaneous lipoma, meningiomyelocele, pilonidal cyst and other inflammatory condition in sacrococcygeal area can easily be made out clinically and histologically. However, there is a case of hamartoma consisting of heterotrophic brain tissue like in our case of newborn that supports the diagnosis.
Myxopapillary ependymomas may arise in the sacrococcygeal region as a primary subcutaneous tumor. On rare occasions, these may be found outside the central nervous system. More than 50 cases have been reported as posterior sacral or subcutaneous region mass [9]. Subcutaneous sacrococcygeal myxopapillary ependymomas grow slowly and therefore are often large and have late presentation. Meckel in the nineteenth century first described a very rear congenital anomaly fetus in fetu. In 1953, Willis [10] made the diagnostic criteria saying fetus in fetu should have vertebral axis with surrounding organs and limbs. This baby girl presented early with the mass at the time of birth and did not have vertebra or long bones. In our case there was presence of only mature brain tissue.
Despite the rarity of heterotopic brain tissue and the nonspecificity of imaging findings, and negative tumor markers, this should be considered in the differential diagnosis of a sacrococcygeal mass.
Conflict of interest statement
None declared.



