-
PDF
- Split View
-
Views
-
Cite
Cite
Peep Talving, Mariliis Rauk, Liisa Vipp, Karl-Gunnar Isand, Aleksandr Šamarin, Kalle Põder, Indrek Rätsep, Sten Saar, Necrosis of the tail of pancreas following proximal splenic artery embolization, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw087, https://doi.org/10.1093/jscr/rjw087
Close - Share Icon Share
Abstract
The current case report presents a rare complication of a significant pancreatic tail necrosis following proximal splenic artery embolization in a 32-year-old male patient involved in a motorcycle accident. Proximal angiographic embolization of the splenic injury after trauma is a widely accepted method with excellent success rate; however, possible complications may occur and has been described in the literature. Nevertheless, only a few case reports pertinent to clinically significant pancreatic tail necrosis after the SAE has been reported. Thus, we add a case report to the scarce literature pertinent to this detrimental and rare complication.
Introduction
Only a few case reports pertinent to clinically significant pancreatic tail necrosis after the splenic artery embolization exist. Thus, we add a case report to the scarce literature describing this rare complication.
Case report
A 32-year-old male was admitted after a high-speed motorcycle accident. Per Emergency Medical Services report the patient had a patent airway, adequate breathing, normal hemodynamics, and a Glasgow Coma Scale score of 15 on the scene of injury. During the transportation, additional O2 at flow rate of 6 l/min per face mask was provided and the patient was resuscitated with 500 ml and 500 ml of crystalloid and colloid, respectively.
The patient was transported to the Emergency Department 65 minutes post injury in a stable condition with a left flank ecchymosis and tenderness over the left thoracoabdominal region. The focused assessment of sonography for trauma depicted perisplenic- and pelvic free fluid. Chest X-ray was normal. The baseline blood count depicted a hemoglobin level at 158 g/l and a positive blood alcohol screen at 2.44 g/l.
After the secondary survey, the patient was subjected to a computed tomography (CT) study, which showed a Grade IV splenic injury per the American Association for the Surgery of Trauma injury grading score with contrast extravasation (Fig. 1), a lower lobe contusion of the left lung, fractures of the IV and VI–XI ribs on the left side and bilateral iliac wing fractures. The pancreatic parenchyma was well perfused and homogenous in a portal venous phase CT-imaging (Fig. 2).
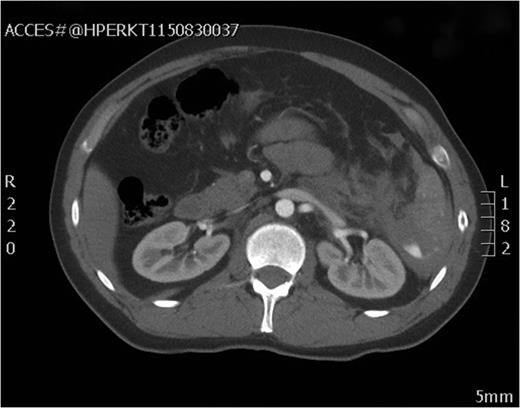
Axial view of the initial CT scan showing Grade IV splenic injury with contrast pooling in the peritoneal cavity.

Axial view of the initial CT scan depicting a normally perfused pancreatic tissue.
After the CT study, angiographic embolization of the splenic artery was performed. Angiographic catheter was inserted through the right femoral artery and guided into the splenic artery through the celiac trunk. The Spongostan (Ethicon Inc., Somerville, NJ, USA) particles were deployed to the branches of the splenic artery as the contrast leakage was seen in multiple locations. The proximal SAE with three Gianturco coils (Cook Medical Inc., Bloomington, IN, USA) and one Azur Peripheral HydroCoil (Terumo Medical Corporation, Somerset, NJ, USA) were deployed 4 cm distal to the celiac trunk (Figs 3 and 4). After the procedure, the patient was admitted to intensive care unit.
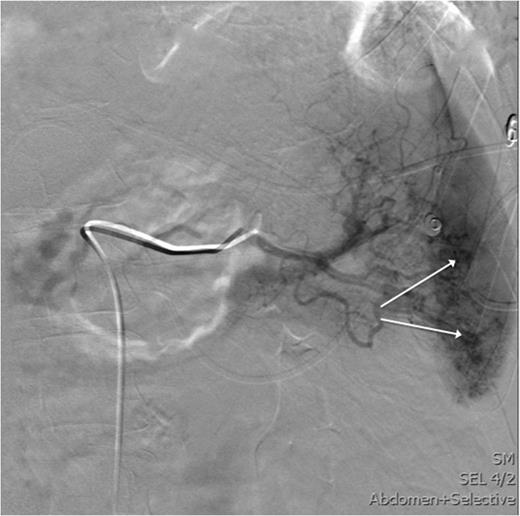
This image shows an angiography of the splenic artery observing splenic contrast leak (white arrows).

Angiographic imaging post-embolization observing four proximal coils in the splenic artery 3–4 cm distal to the celiac trunk.
On the following day the patient experienced an intense abdominal pain, tachycardia and distress and was studied with a follow-up CT scan observing distal pancreatic ischemia (Fig. 5). As the clinical exam was consistent with peritonitis the patient was subjected to exploratory laparotomy. Similar to the CT findings, an obvious distal pancreatic ischemia was noted during surgery (Fig. 6). Distal pancreatectomy with splenectomy was performed. The pancreatic stump was oversewn and a 30 F drain was placed at the pancreatic resection margin.
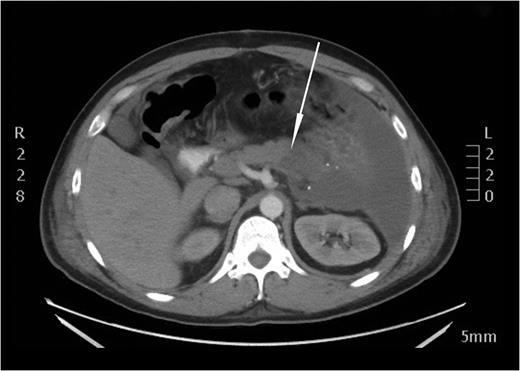
An axial CT image performed on the next day after embolization. A distinct perfusion discrepancy between a normally perfused body and a non-perfused tail of the pancreas is noted (white arrow).
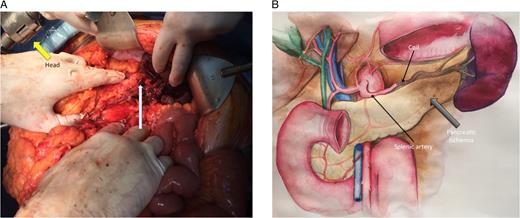
(A) The photo shows the intraoperative finding with distal pancreatic ischemia (white arrow). (B) The same intraoperative finding depicted on the illustration. Most of the stomach is removed on the illustration (illustration by Getter Laur).
The post-operative course was complicated with three adverse events per Clavien–Dindo [1]: intra-abdominal abscess (Grade IIIa), pleural effusion (Grade IIIa) and a high-output pancreatic fistula (Grade IIIa) requiring octreotide administration. Patient was discharged on the 22nd post-operative day in a good condition.
Discussion
The non-operative management (NOM) of hemodynamically stable patients with splenic injuries is a widely accepted strategy with excellent outcomes [2]. Also, angioembolization of high-grade splenic injuries have shown good outcomes with significantly increased success rates of NOM [3]. Several techniques of splenic embolization exist: proximal, distal, and their combination with coils and/or spongostan particles. The proximal embolization does not directly terminate bleeding but rather enables clot formation by decreasing perfusion pressure to the spleen. However, a distal embolization aims to arrest the hemorrhage directly by reducing blood flow at the bleeding source [4].
While splenic artery embolization is increasing in frequency, more investigators have reported complications associated with embolization techniques. In a meta-analysis by Schnüriger et al. [5], pooled patient outcomes were compared in proximal and distal splenic embolization. The most frequent complication observed was splenic infarction, being significantly higher after distal embolization. Other frequent adverse events were splenic re-bleeding and infectious complications that did not differ between the techniques. However, only a few scientific reports on clinically relevant pancreatic tail necrosis after SAE exist. Khurana et al. [6] reported a case pertinent to a 54-year-old male who was involved in a motor vehicle accident with CT scan depicting a splenic injury without associated injuries. The SAE was performed resulting in severe abdominal pain and distension two days after the procedure. A follow-up CT scan revealed necrosis of pancreatic tail and a laparotomy was performed with a splenectomy and distal pancreatectomy. Likewise, Paul et al. [7] reported two cases of distal pancreatic necrosis following proximal splenic artery embolization, which led to distal pancreatectomy. Also, in a case report by Hamers et al. [8] a pancreatic necrosis occurred after proximal SAE; however, this patient was managed non-operatively.
All the cases reported have a similar course with significant abdominal pain coherent with peritonitis few days after proximal embolization due to the distal pancreatic necrosis [6–8].
Pancreatic tail receives perfusion mainly from the splenic artery through many branches. Two largest branches are the dorsal pancreatic artery and the greater pancreatic artery arising from the middle segment of the splenic artery [9]. Thus, when proximal embolization is performed, a risk of ischemic insult of the pancreatic tail is conceivable; however, only a few case reports are available in the literature and the extent of ischemic insult in these instances may vary with individual anatomic vascular variations. Also, some authors have proposed that proximal embolization accompanied by a splenic hilar hematoma or microvascular injuries, not evident on a CT scan, may potentially increase the risk for distal pancreatic ischemia [10]. The clinical associations between proximal SAE and pancreatic tail necrosis have certainly gone unrecognized prior to the emerging cases in the contemporary literature.
In conclusion, this report presents a case of distal pancreatic necrosis after proximal splenic embolization, being a severe and a rare adverse event, which often leads to surgery and complicated post-operative course. While splenic embolization is becoming a gold standard treatment in hemodynamically stable splenic injuries, the appreciation of this complication may ensure prompt diagnosis and treatment of the condition. However, for definite conclusions, more reports are warranted.
Conflict of Interest Statement
None declared.



