-
PDF
- Split View
-
Views
-
Cite
Cite
Katherine J. L. Suter, Niruben Rajasagaram, Peter Nottle, Gastric band connection tube results in small bowel obstruction: an acute emergency, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw082, https://doi.org/10.1093/jscr/rjw082
Close - Share Icon Share
Abstract
The laparoscopic adjustable gastric band (LAGB) is a widely performed procedure for the morbid obesity epidemic. Despite its low mortality compared with other mainstream bariatric surgeries, it is not without its complications. The authors report a late and rare complication of a small bowel obstruction in a 52-year-old woman from an LAGB placed for 2 years. She was diagnosed clinically and radiologically with a small bowel obstruction. However, in the setting of an LAGB, this became a closed-loop obstruction. She proceeded to an emergency laparoscopy, which revealed that the port connection tube had formed dense adhesions to the jejunum causing an obstructive band. This is only the fifth reported case in Australia; as bariatric surgery continues to rise, these patients may present unannounced to any emergency department and as such should be treated as a closed-loop obstruction with immediate resuscitative and surgical management instituted.
INTRODUCTION
The pandemic of obesity is one of the greatest public health risks in industrialized countries. In Australia, for instance, the prevalence of obesity (body mass index >30) has more than doubled in the past 25 years [1]. Bariatric surgery is now proven to be the most effective means of achieving sustainable weight loss from a condition that has been highly resistant to dietary, lifestyle and pharmacological interventions [2].
The laparoscopic adjustable gastric band (LAGB) even though decreasing in its popularity has in the past been among the most frequent preferred bariatric procedures in many western countries due to its success in achieving weight loss with the lowest mortality rate among all bariatric procedures [3]. Despite this, it is not without its complications. The authors report a late and rare complication of a small bowel obstruction (SBO) caused by the connection tube placed in an LAGB 2 years earlier, interestingly with initial negative clinical and radiological findings on the patient’s first presentation.
CASE REPORT
This case examines a 52-year-old woman who initially presented to the emergency department with a 2-week history of vague abdominal pain. She had been privately investigated 1 week earlier for this pain with a negative computed tomography scan and gastroscopy. The patient’s history did not suggest any of the usual alarm symptoms associated with LAGB patients and neither did the clinical examination reveal significant findings. The impression was that of a port site infection, and she was discharged home with a script for cephalexin and follow-up in the outpatient clinic.
Two weeks later, she re-presented to the emergency department with a 24-hour history of severe central abdominal pain associated with vomiting and multiple episodes of loose stools. On examination, she was found to be hypotensive, tachycardic and peritonitic. The suspicion of an SBO was established by plain film radiograph appearances with multiple air fluid levels and distended bowel loops (Fig. 1). Computed tomography scan of the abdomen and pelvis showed the transitional zone to be in mid abdomen (Fig. 2). This was thought to be most likely secondary to adhesions. She proceeded on to have an emergency laparoscopy. Interestingly, the laparoscopy identified the transition point of the SBO to be an adhesion formed between the LAGB tube, the mid jejunum and the stomach forming a classic closed-loop obstruction (Fig. 3). The laparoscopic division of this adhesion was performed successfully. The rest of the small bowel was run along its entire length with no other transition point found. The adjustable gastric band was removed at the same time along with the associated port. Postoperatively, she had an uncomplicated recovery and was discharged on Day 4 post-admission without further sequelae.

SBO established on plain abdominal radiograph, with gastric band tubing and port also evident.
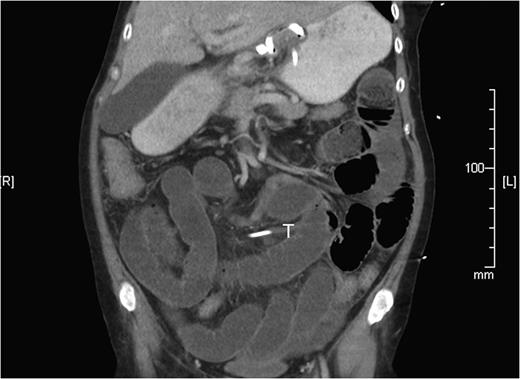
Computed tomography reconstruction showing the SBO with transition zone in the mid ileum, later discovered to be caused by gastric band tubing (T).
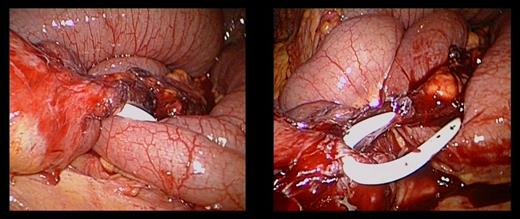
The gastric band connection tube had formed a dense adhesion to the jejunum resulting in a tight obstructive band.
DISCUSSION
LAGB has been a very popular choice in Australia for bariatric surgery. While LAGB is considered one of the safest due to its almost complete reversibility and preservation of gastrointestinal tract continuity [4], there are potential complications that could be life threatening that require early diagnosis and prompt surgical intervention. Interestingly, most long-term follow-up studies have not highlighted SBOs related to connection tubes as frequent complications or at all [4, 5]. As more patients with LAGBs present to our emergency department, it will be important to create a diagnostic algorithm to alert the various treating medical specialists to their potential complications [6], keeping in mind the connection tube as a causative factor.
Traditionally, the length of the connecting tube is preserved for two reasons: (i) to facilitate revision surgery in cases of infection and (ii) to prevent tension on the band from the anterior abdominal wall [7]. Mills et al. [8] eluded to the long length of the tube being a causative factor for these SBO. In the course of great weight loss, the distance traversed by the tube from the stomach to the abdominal wall becomes significantly altered, thus leaving much of the length of the original tube redundant. Others have addressed the redundant tube by electing to suture the tube to the anterior abdominal wall above the liver in an attempt to prevent future obstructions [9, 10]. Whether this should become a routine procedure intraoperatively or post-significant weight loss remains to be explored.
The current treatment of managing patients with SBO who present after undergoing surgery is to observe with a trial of conservative management. This, however, should not be the default position for patients who present with an SBO and an adjustable gastric band in-situ. This creates a closed-loop obstruction and if not recognized and dealt with urgently can result in serious consequences.
The increased specialization of surgeons in advanced laparoscopy has made a laparoscopic approach the preferred method of primary management. The presence of dilated loops of small bowel makes this technically challenging but very much one that would be within the capability of this generation of surgeons. The success of performing this operation with minimal invasive surgery would be partly dependent on the patient’s systemic factors as well as the familiarity of the treating surgeon with managing complications from bariatric surgery. Nonetheless, in an acute setting of paramount importance would be to relieve the obstruction regardless of being with laparoscopic or open surgery.
CONCLUSION
Most complications related to LAGB in obesity surgery are non-life threatening, but importantly they often have a nonspecific clinical history and examination, as was demonstrated in our case report. This is only the fifth reported case of a connection tube causing an SBO in Australia: as bariatric surgery continues to rise, these patients may present unannounced to any emergency department. Although not a common complication, one that could easily see the safety record of LAGB patients tarnished if this small subgroup of patients is not acted upon promptly by emergency departments’ unfamiliar LAGB surgery. As such, we place importance on familiarizing oneself with single-case studies or series in bariatric complications to be able to recognize those surgical emergencies when they present often years after their primary procedure [6].
Conflict of interest statement
None declared.



