-
PDF
- Split View
-
Views
-
Cite
Cite
Hasan Raza Mohammad, Anand Pillai, Limb salvage talectomy for 3C Gustilo–Anderson fracture, Journal of Surgical Case Reports, Volume 2016, Issue 5, May 2016, rjw081, https://doi.org/10.1093/jscr/rjw081
Close - Share Icon Share
Abstract
Foot fractures vary in severity with complex midfoot fractures having poor morbidity rates and high amputation rates. Complex midfoot fractures are rarely reported since they are uncommon and only treated in specialist centres. Given the important role of the midfoot in foot function, reconstruction is preferable. Soft tissue management on the dorsal aspect of the foot poses further challenges to reconstructive surgeons. We report a case of a 55-year-old woman who sustained an open 3C Gustilo–Anderson fracture that was initially treated with open reduction internal fixation and free flap. She subsequently developed flap and internal fixation failure with osteomyelitis of the talus. We report a good outcome using primary limb shortening with a talectomy, tibiocalcaneal arthrodesis using external fixation and a combination of vancomycin-loaded calcium sulphate and intravenous antibiotics in our patient.
INTRODUCTION
We report a case of a patient who presented with a complex open 3C Gustilo–Anderson fracture who subsequently developed flap failure, failed internal fixation complicated with osteomyelitis of the talus.
Foot fractures are relatively common contributing to 12.3% of all fractures [1]. They vary in severity from minor metatarsal/phalangeal fractures to complicated midfoot and hindfoot injuries. Open fractures are poorly reported since they are rare and usually treated in specialist trauma centres. Reported amputation rates in open midfoot fractures are 30% highlighting their severity, coexisting soft tissue compromise, infection and difficulty covering midfoot injuries with flaps [1]. With the midfoot playing a key role in foot function, reconstruction rather than amputation is preferable. Soft tissue defects of the foot pose further challenges given the specially adapted architecture to facilitate tendon gliding.
CASE REPORT
A 55-year-old woman presented with an open 3C Gustilo–Anderson fracture. Her medical history included rheumatoid arthritis, osteoarthritis, ischaemic heart disease, diabetes mellitus and asthma. Soft tissues were closed using a free flap from the left thigh and a flap from the right lower limb. Bony injury was treated with open reduction internal fixation with screw fixation of the first and third metatarsals into the talus with restoration of the medial and middle columns achieved using cannulated screws. Additional stability was achieved by plate fixation of the medial and lateral columns (Fig. 1). The treatment was deemed successful, and the patient was discharged.
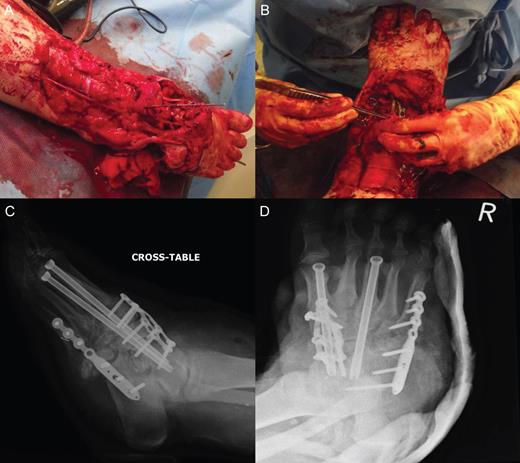
Open 3C Gustilo–Anderson injury. (A and B) Theatre images of open 3C Gustilo–Anderson fracture. (C and D) Radiographs illustrating open reduction internal fixation (ORIF) (screw fixation of the first and third metatarsals into the talus). The ORIF using cannulated screws allowed restoration of the medial and middle columns of the foot. Plate fixation of the medial and lateral column was conducted to achieve additional stability.
Four months since the initial presentation, she was readmitted due to foot dorsal flap edge failure for which vacuum-assisted closure was unsuccessful (Fig. 2). The patient’s C-reactive protein was 63 mg/l with normal white cells. An angiogram revealed complete occlusion of the anterior tibialis and dorsalis pedis arteries.

Flap failure on dorsal aspect of foot when patient presented after failed vacuum-assisted closure treatment.
Wound debridement demonstrated pus at screw insertion sites with navicular and talar involvement. The patient had inadequate soft tissue coverage, bony osteomyelitis and necrotic bone. Primary limb shortening with a talectomy was conducted to reduce the soft tissue deficit and remove infected and necrotic bone, tibiocalcaneal arthrodesis for joint stability using external fixation, and dead space was treated with calcium sulphate mixed with vancomycin and systemic intravenous and oral antibiotics for osteomyelitis postoperatively (Figs 3 and 4). The wound was closed after the external fixator was applied. Wound swabs and bone samples revealed Enterococcus faecalis and E. raffinosus and diphtheroids. The patient was treated with intravenous teicoplanin and meropenem with oral stepdown to linezolid and ciprofloxacin.
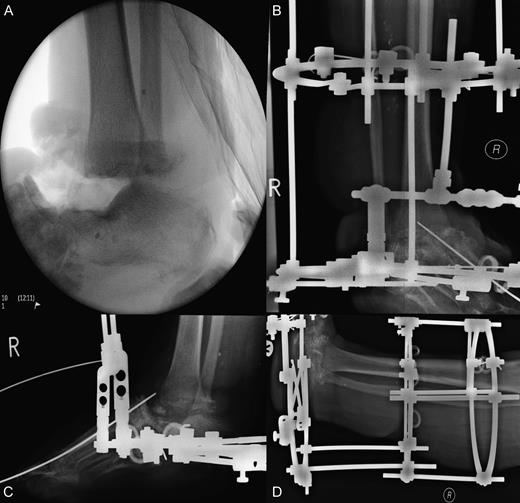
Surgical images of talectomy and external fixation used for tibiocalcaneal arthrodesis. (A) Anterior posterior intraoperative radiograph illustrating talectomy. (B–D) Radiographs showing external fixation in situ.
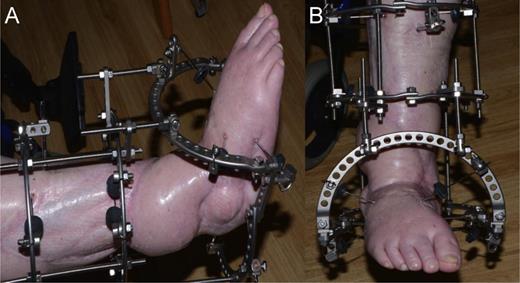
External fixation used to facilitate tibiocalcaneal arthrodesis post talectomy. (A) Lateral view (B) Anterior posterior view.
Eight months since the initial presentation, the patient was taken to the theatre where a large defect in the anterior dorsum of the foot, and the external fixator was adjusted in the foot to allow for exploration and debridement. Secondary reconstruction was performed. The abductor hallucis was identified and the tendon divided distally and mobilized and rotated to fill in the soft tissue medial defect. Calcium sulphate with vancomycin and gentamycin was inserted into the bony defect, and external fixation frame was adjusted back to its original position. The wound was closed using the abductor hallucis and skin graft from the right lateral leg. Postoperatively the patient was put on intravenous teicoplanin and meropenem with oral stepdown to linezolid and ciprofloxacin. On discharge once the infection was controlled the patient’s CRP was 6.0, white cell count 7.9 and neutrophils 4.0.
After having the external fixation for 8 months in total, it was removed when fusion was deemed adequate on computed tomography imaging (Fig. 5). She was instructed to weight bear while in a plaster of paris cast for 14 days and then a moon boot for 14 days. Two months after this, the patient was mobilizing without issues and was doing well. At 12 months, the patient stated that she is able to mobilize with any mild residual pain controlled with analgesia.
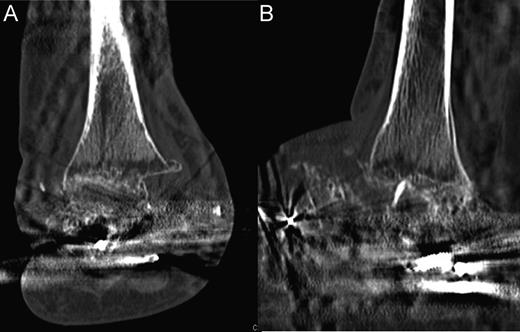
Computed tomography scans illustrating tibiocalcaneal fusion 1 year postoperatively. (A) Anterior–posterior view; (B) Lateral view.
DISCUSSION
Midfoot injuries with talar infections can often lead to below-knee amputation with the main goals of treatment being to successfully treat the infection and maintain a functional foot. In adults, usually a talectomy is required to eradicate the infection [2, 3]. Talectomy is usually performed with tibiocalcaneal arthrodesis to achieve joint stability [4].
Few reports of the isolated use of external fixation in complex foot injuries exist [5]. Most work focuses predominantly on internal fixation techniques or a combination of internal and external fixation. Most reports of arthrodesis following talectomy are for patients with Charcot deformities rather than traumatic injuries with osteomyelitis [5]. To successfully treat patients with infected midfoot injuries, biomechanical stability and eradication of the infection is essential.
Calcium sulphate with antibiotics was used intraoperatively in the fusion site with some evidence supporting its use in deep foot infections [6]. Following this, a long course of intravenous antibiotics was used according to the sensitivities of the microorganisms growing in the region.
Biomechanical multiplanar stability was achieved using case external fixation. External fixation facilitates soft tissue healing, allows earlier weight bearing, closer monitoring of surgical incision sites and postoperative adjustments [5].
There are mixed reports whether external fixation suffices independently in facilitating tibiocalcaneal arthrodesis. Fabian and colleagues [7] concluded that tibiocalcaneal fusion in seven Charcot joint patients using external fixation alone was unlikely to lead to fusion but the fibrous healing was sufficient. Agarwala’s group and Dennison’s group report full fusion in all of their patients undergoing arthrodesis using external fixation [8, 9].
Our results are in concordance with work of Agarwala and Dennison et al. in that external fixation is sufficient in achieving tibiocalcaneal arthrodesis. There is a need for randomized controlled trials to investigate the most appropriate fixation technique for tibiocalcaneal arthrodesis.
In conclusion, we report a good outcome treating an open 3C Gustilo–Anderson fracture complicated by osteomyelitis, necrosis and inadequate soft tissue coverage. Our management involved a single-staged talectomy to remove the infected bone and tackle the inadequate soft tissue coverage, external fixation for tibiocalcaneal arthrodesis to achieve joint stability and a combination of bone graft antibiotics and a course of intravenous and oral antibiotics postoperatively to deal with the underlying osteomyelitis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- vancomycin
- amputation
- fractures
- calcium sulfate
- limb
- fracture fixation, internal
- limb salvage
- osteomyelitis
- reconstructive surgical procedures
- talus
- external fixation devices
- foot
- morbidity
- open reduction with internal fixation
- foot fractures
- midfoot
- free flap
- midfoot fracture
- antibiotic therapy, intravenous
- arthrodesis
- talus excision
- soft tissue



