-
PDF
- Split View
-
Views
-
Cite
Cite
M. Tarazi, N. Mayooran, B. Philip, M.N. Anjum, K. O'Regan, K. Doddakula, Anomalous right upper lobe venous drainage, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw043, https://doi.org/10.1093/jscr/rjw043
Close - Share Icon Share
Abstract
Lung resections are usually not associated with significant bleeding, but can be fatal, especially in cases of video-assisted thoracoscopic surgery (VATS). Anomalous vascular structures could be a major reason for unexpected bleeding in such surgeries. We present a case of an aberrant upper lobe pulmonary vein that was encountered posterior to the right upper lobe bronchus during a right upper lobectomy via thoracotomy. The anomalous pulmonary vein was identified preoperatively on a computed tomography (CT) scan and hence was looked for before dividing the bronchus. Many centres are adopting the VATS approach for performing lung resections. If an anomalous vein is present posterior to the bronchus, it might be in a blind spot and could be damaged inadvertently, leading to profuse and potentially fatal bleeding. We conclude that the identification of anomalous vascular structures prior to surgery with the help of CT helps in avoiding adverse outcomes.
INTRODUCTION
Significant bleeding during formal lung resection is rarely encountered, but can be a fatal life-threatening possibility. With the increased use of video-assisted thoracoscopic surgery (VATS) in lung resections, it becomes even more important to identify any anomalous vascular structures to avoid fatal bleeding. We present a case of right upper lobectomy in which an aberrant right upper lobe pulmonary vein was encountered posterior to the right upper lobe bronchus draining to the left atrium detected preoperatively on review of the patient's computed tomography (CT) scans.
CASE REPORT
A 53-year-old male patient was referred to our surgical services with a biopsy-proven adenocarcinoma of the right upper lobe. During an admission to the hospital with diarrhoea, a CT thorax was performed showing an incidental finding of a ground glass nodule in the right upper lobe, which was found to be PET-positive with an SUV of 1.9. This gentleman's past medical history was significant for global immune deficiency syndrome on monthly immunoglobulin infusions, haemochromatosis, ischaemic heart disease and peripheral vascular disease with previous bilateral femoral bypass. Of note, this patient was an ex-smoker who quit 4 weeks prior to the surgery.
Pulmonary function tests: FEV1 3.3 l (96%), FVC 3.7 l (89%), FEV1/FVC 89%, DLCO 56%.
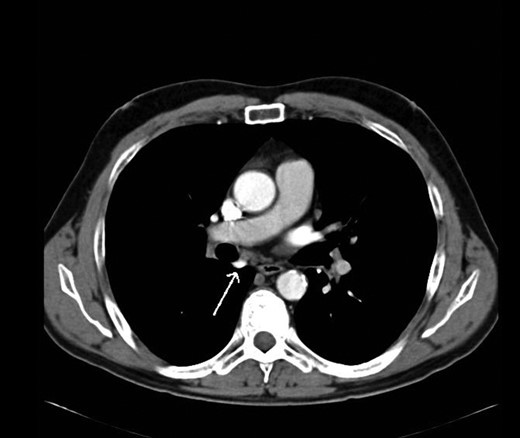
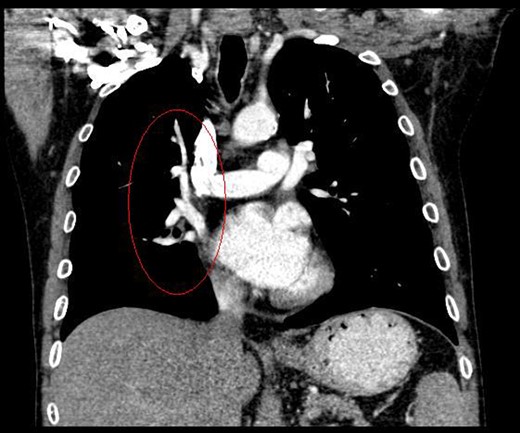
During discussions at the multidisciplinary team meeting, the computed tomography scans of his thorax were reviewed by our radiology colleagues and an anomalous right upper lobe vein was identified.
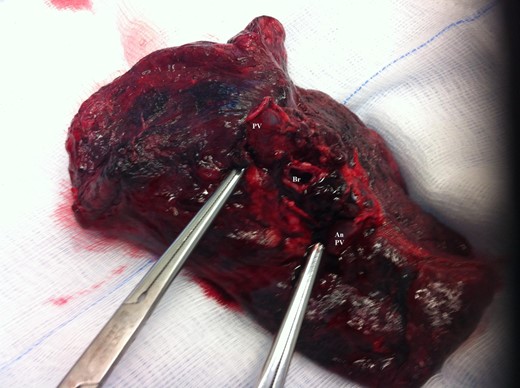
The patient underwent a right postero-lateral thoracotomy. The right upper lobe pulmonary artery and vein were identified and divided with vascular Endo GIA™ staples. Lymphadenectomy was performed in the draining lymph nodes and we proceeded to isolate the upper lobe bronchus. Prior knowledge of an anomalous venous drainage of the upper lobe made us adopt a cautious approach during dissection posterior to the right upper lobe bronchus and a vascular structure was identified that could be traced in the left atrium; thus, it was found to be an anomalous upper lobe pulmonary vein. The anomalous vein was divided with vascular Endo GIA™ staples. The bronchus was divided with a TA™ stapler.
The patient recovered well postoperatively and was discharged home. Histologically, the patient's tumour stage was pT1aN0 (Figs 1–6).



DISCUSSION
Pulmonary vascular variations are associated with a potential risk of bleeding during pulmonary resections. The preoperative identification of these vascular variations is vital for the safe and proper resections in thoracic surgery [1].
Kim et al. [2] first reported the contrast-enhanced computed tomography findings of aberrant pulmonary veins, which were observed as a focal nodularity attached to the posterior wall of the bronchus intermedius. Pulmonary vein variations are usually seen in the common pulmonary vein and the middle lobe vein draining into the inferior pulmonary vein or the left atrium [3]. There are only a few CT studies of the upper lobe vein. The frequency is reported between 1.7 and 5.7% [3].
Kim et al. [2] eluded that in 5% of normal subjects, the right superior segmental pulmonary veins had an aberrant course also either to the inferior pulmonary vein or directly to the left atrium. Asai et al. [4] noted that in right lung resection surgeries, there was a 5.7% occurrence of abnormal right upper lobe venous drainage.
Recent advances in non-invasive imaging methods such as multi-detector computed tomography and magnetic resonance angiography have facilitated the detection of pulmonary vessels [4]. Watanabe et al. and Usami et al. reported that three-dimensional CT angiography is a far less invasive and an easier method for delineation of pulmonary vessels than conventional pulmonary angiography prior to lung resection [1].
Open thoracotomy lung resection has the advantage of having a three-dimensional view of the operative field compared with the two-dimensional view in video-assisted thoracoscopic lung resections. The surgeon uses both visual and tactile inputs to confirm the anatomy of the organs; however, with thoracoscopy, there is less tactile input [5].
Hence, our case demonstrates that it is prudent to identify anomalous vascular structures which may be damaged while performing lung resection.
Many centres are adopting the VATS approach when performing lung resections. This is gradually getting recognized as a standard practice. In VATS resections, the relevant bronchus is divided after the stapling and division of the pulmonary veins but prior to the stapling and division of the pulmonary arteries in that lobe. In such cases, if an anomalous vein is present posterior to the bronchus, it might be in a blind spot and could be damaged inadvertently, leading to profuse and potentially fatal bleeding.
We conclude that the identification of anomalous vascular structures prior to surgery with the help of CT helps in avoiding adverse outcomes.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
CONFLICT OF INTEREST STATEMENT
None declared.



