-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroyoshi Tsubochi, Shunsuke Endo, Kentaro Minegishi, Tetsuya Endo, Superior vena cava repair with left brachiocephalic vein flap, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw015, https://doi.org/10.1093/jscr/rjw015
Close - Share Icon Share
Abstract
Interposition with a vascular prosthesis or patch closure using autologous pericardium has been applied for superior vena cava (SVC) reconstruction during surgery for thoracic malignancies such as thymic epithelial tumors or lymphadenopathy that invade the SVC. We herein report a novel and simple method for repair of the SVC using a left brachiocephalic vein flap. This procedure is useful to repair the anterior wall of the distal portion of the SVC, which is a common site of invasion of thoracic malignancies.
INTRODUCTION
Combined resection of the superior vena cava (SVC) is sometimes required during surgical treatment of mediastinal tumors and lymph node metastasis from lung cancer, and several reconstructive methods of the SVC have been described [1]. We herein propose a novel and simple technique for repair of SVC wall defects using a left brachiocephalic vein flap.
CASE REPORT
Case 1
A 33-year-old man was referred to our hospital because of abnormal chest shadow. Contrast-enhanced computed tomography (CT) revealed a 50-mm-diameter mass in the anterior mediastinum (Fig. 1). Invasion of the anterior wall of the SVC was suggested because of the unclear border between the tumor and the SVC. 18F-Fluorodeoxyglucose uptake on positron emission tomography exhibited a maximum standardized uptake value of 6.5. From radiographic findings, the mass was suspected to be a malignant tumor such as a thymoma or thymic cancer, although a pathological diagnosis was not established. Therefore, we planned extirpation of the tumor via a median sternotomy.

Contrast-enhanced CT showing an anterior mediastinal tumor with suspected invasion of the SVC.
Exploration revealed a solid mass, which infiltrated the anterior wall of the distal portion of the SVC from the confluence of the bilateral brachiocephalic veins to just above the azygos junction. The left brachiocephalic vein was transected with stapler 40 mm from the brachiocephalic vein junction. After cross-clamping of the SVC at the level above the azygos vein and right brachiocephalic vein, the tumor was extirpated with partial excision of the SVC wall. The SVC wall defect measured 30 × 7 mm. The caudal side of the left brachiocephalic vein was then divided longitudinally, and the pedicled flap of the left brachiocephalic vein was sewn onto the SVC defect using 5-0 Prolene (Ethicon, Somerville, NJ) (Fig. 2A and B). The SVC clamping time was 29 min. Slight swelling of the left arm occurred postoperatively and resolved within 5 days. The postoperative course was uneventful. The tumor was pathologically diagnosed as thymic cancer. Contrast-enhanced CT 1 month postoperatively revealed the patency of the reconstructed SVC.
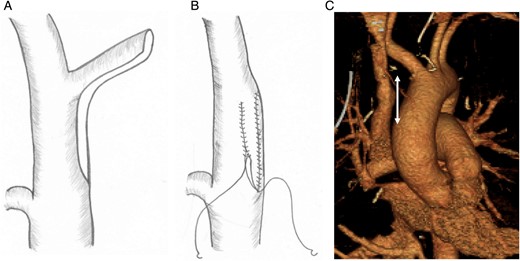
Reconstruction of the SVC with the left brachiocephalic vein. (A) After transection of the distal side of the left brachiocephalic vein with a stapler and extirpation of the tumor with partial resection of the SVC, the caudal side of the left brachiocephalic vein was divided longitudinally. (B) A pedicled flap was then made from the left brachiocephalic vein and sewn onto the SVC defect. (C) Postoperative three-dimensional CT showing patency of the reconstructed SVC. The two-directional arrow indicates the range of repair.
Case 2
An asymptomatic 57-year-old man was diagnosed with right lung squamous cell carcinoma and referred to our hospital for further evaluation and treatment. Contrast-enhanced CT revealed a 45-mm-diameter mass in the lower right lung lobe and a 25-mm-diameter swollen anterior mediastinal lymph node adjoined the anterior side of the SVC. The patient was clinically diagnosed with T2aN2M0 lung cancer. The patient had interstitial pneumonia and elected to undergo surgical resection of the tumor instead of chemoradiotherapy.
Through a posterolateral thoracotomy in the fifth intercostal space, a right middle and lower sleeve lobectomy was performed prior to the lymphadenectomy. An enlarged anterior mediastinal lymph node infiltrated the anterior wall of the SVC. The lymph node was excised with the anterior SVC wall between the brachiocephalic vein junction and the azygos vein junction. The SVC wall defect measured 30 × 7 mm and was covered with a left brachiocephalic vein, as in Case 1. The clamping time of the SVC was 45 min. The postoperative course was uneventful. Patency of the reconstructed SVC was confirmed on contrast-enhanced CT 1 month postoperatively (Fig. 2C).
DISCUSSION
The optimal technique for SVC reconstruction depends on the extent and location of the neoplastic invasion. When SVC infiltration involves >50% of the circumference of the SVC, graft interposition using a ringed polytetrafluoroethylene (PTFE) graft is preferred [2, 3]. If the SVC invasion is <50%, primary suturing can be applied under partial clamping of the SVC [3]. However, primary suturing may cause SVC narrowing and early thrombosis, and insufficient surgical margins may result in residual tumor tissue. Therefore, if more extensive SVC wall resection is required, autologous pericardium is often used to cover the SVC defect [1]. Ohata et al. recently reported another unique method with which to repair the SVC wall defects using an azygos flap [4]. They cut the azygos arch longitudinally on the caudal side to cover the SVC wall defect. Although their method is useful for reconstruction of the posterior side of the SVC near the azygos vein, it seems unsuitable for anterior repair. In contrast, the left brachiocephalic vein flap is useful for repair of the anterior and more distal portions of the SVC which is a common site of invasion of mediastinal malignancies. Transection of the left brachiocephalic vein may cause temporary left arm swelling, but this usually resolves within 1 week. There are some advantages of using the autologous tissue for reconstruction of the SVC. For example, this method can reduce the risk of infection, which is likely to occur when a vascular prosthesis such as a PTFE graft is used. Additionally, postoperative anticoagulation therapy is not necessary. With respect to the surgical approach, a sufficiently long vessel flap can be obtained not only through median sternotomy or hemi-clamshell, but also through lateral thoracotomy by dissecting the left brachiocephalic vein as distal as possible, as in our Case 2.
Total SVC clamping is necessary during this procedure. An SVC bypass is not always essential when the clamping is performed at the level above the azygos vein, as performed in our cases, because some lateral circulation is preserved and cerebral edema can be reduced. However, a temporary extra-anatomic venous shunt is usually required when clamping is performed below the azygos vein for >60 min [1].
In conclusion, SVC reconstruction using a left brachiocephalic vein flap is a simple and useful method when SVC invasion is limited to the anterior wall of the distal portion and involves <50% of the circumference. This technique can prevent narrowing or early occlusion of the SVC, which may occur after primary suturing, and postoperative anticoagulant therapy (essential for PTFE grafting).
CONFLICT OF INTEREST STATEMENT
None declared.



