-
PDF
- Split View
-
Views
-
Cite
Cite
Nina Kolbe, Kathleen Sisson, Renato Albaran, Abdominal pain and hematuria: duodenal perforation from ingested foreign body causing ureteral obstruction and hydronephrosis, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw018, https://doi.org/10.1093/jscr/rjw018
Close - Share Icon Share
Abstract
Foreign body (FB) ingestion is a relatively common reason for visits to the emergency room. If the FB is symptomatic or damaging to the patient, either endoscopic or surgical intervention should ensue. We present a case of abdominal pain and hematuria beginning ∼24 h after an incidental FB ingestion. Initial CT imaging defined a linear opacity perforating through the posterior duodenal wall abutting the ureter causing inflammation and hydronephrosis. After two unsuccessful endoscopic attempts at retrieval, we were able to identify the object with the aid of intraoperative fluoroscopy and surgically remove the FB. The patient recovered uneventfully and was discharged home. Posterior duodenal perforation by an FB may not manifest with obvious localized or systemic symptoms unless the perforation involves surrounding structures such as the aorta, vena cava or ureter. In such cases, surgical intervention is required for FB removal.
INTRODUCTION
Foreign body (FB) ingestions in the adult population are frequently incidental and the majority can successfully be removed endoscopically [1, 2]. Patients with prolonged impaction (over 12 h) and those who ingested sharp-pointed objects have a greater risk of complications [2]. The jejunum and ileum are most commonly involved with perforations. Perforations of the duodenum are relatively rare (5–10%) and present in a more innocuous manner [3]. In cases of duodenal FB perforation into adjacent structures, surgical retrieval is necessary [4].
CASE REPORT
A 38-year-old male presented to the hospital with a chief complaint of abdominal pain and hematuria 1 day after eating a barbecue pulled pork sandwich. He described the pain as ‘deep’ in his abdomen, sharp and non-radiating with no episodes of nausea, emesis or diarrhea. He denied any dysuria or frequency. The patient's past medical and surgical history was unremarkable. He had no abnormalities on his laboratory values besides a urinalysis demonstrating 2+ blood and 11–24 RBCs/hpf. Physical examination revealed point tenderness to deep palpation to the right of his umbilicus, but his abdomen was soft with no signs of peritonitis. An upright abdominal X-ray was unremarkable; however, a CT of his abdomen demonstrated a 2-cm linear density representing the FB in the posterior third portion of the duodenum perforating into the retroperitoneum abutting the right ureter causing hydronephrosis (Figs 1 and 2, arrow). Two separate attempts were made at endoscopic retrieval in the first 24 h without successful visualization or removal of the FB. Due to the ureteral involvement and hydronephrosis, an operative intervention was recommended.
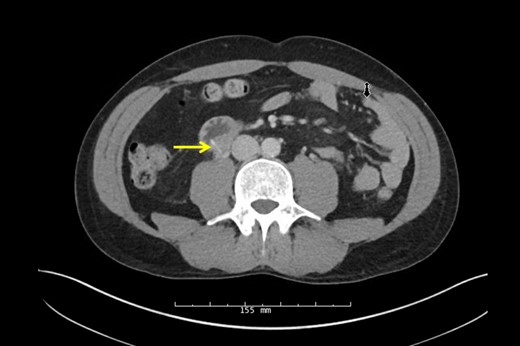
CT scan of linear opaque FB traversing the posterior wall of the duodenum abutting the ureter.

Sagittal CT scan again demonstrating the FB through the posterior wall of the duodenum onto the anterior surface of the ureter.
Urology performed a right retrograde pyelogram demonstrating a point of obstruction in the proximal ureter with no contrast extravasation. A guide wire and stent were passed through the obstruction into the hydronephrotic right kidney without difficulty. Following successful stent insertion, fluoroscopy was used to confirm the location of the FB at the junction of the second and third portion of the duodenum. A full Kocher maneuver was performed and the duodenum and ureter were separated. A small, linear, FB was identified projecting from the posterior third portion of the duodenum into the ureter (Fig. 3) and extracted without injury (Fig. 4). The patient's original abdominal pain resolved after the surgery. He was able to tolerate a diet and be discharged on postoperative day 4.
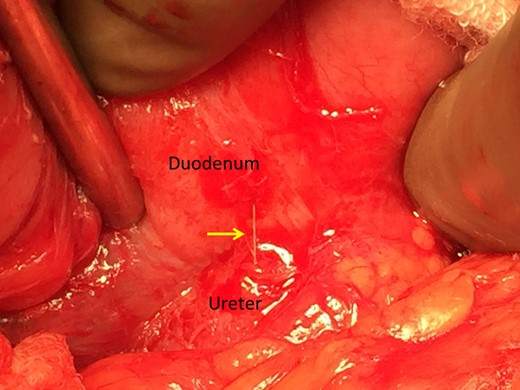
Intraoperative identification of the FB from the duodenum to the ureter.

Pathology confirmed a wire metal bristle, likely from a grill brush.
DISCUSSION
Roughly half of all patients with FB ingestion are unaware of swallowing the object at the time of consumption. A literature review on accidental toothpick ingestion by Steinback et al. [5] reported that 54% of patients were unaware of having swallowed a toothpick and 23% of toothpicks were localized to the duodenum. Duodenal perforations do not lead to peritonitis if perforation into the retroperitoneum occurs; however, in this location, the toothpick may migrate into adjacent retroperitoneal structures (i.e. ureter).
There are few other case reports of FB ingestion leading to duodenal perforation and hydronephrosis. In one case, incidental toothpick ingestion presented with symptoms mimicking renal colic. The toothpick perforated and fixed in the duodenal wall between the second and third duodenal portions causing inflammation and hydronephrosis [6]. In another case, the patient presented with abdominal pain and hematuria, similar to our case due to a toothpick ingestion perforating the duodenal wall into the right kidney. Endoscopic extraction was unsuccessful because the toothpick had migrated out of the duodenal lumen and exploratory laparotomy with surgical removal was required [7].
The most common site of perforation in the gastrointestinal tract is the ileum, with rates from 18 to 66% [3, 5, 8]. Duodenal injury occurs with FB ingestion 10% of the time with a complication rate three times higher than other gastrointestinal tract locations [9]. The majority of perforative complications occurred in the second portion of the duodenum. Ideally, endoscopic retrieval of the FB is the treatment of choice for objects located in the first and second portion of the duodenum [10]. Once objects migrate distally into the third portion of the duodenum, however, patients may experience complications such as perforation into a retroperitoneal organ and surgical intervention must ensue.
CONFLICT OF INTEREST STATEMENT
None declared.



