-
PDF
- Split View
-
Views
-
Cite
Cite
Ikennah L. Browne, Elijah Dixon, Delayed jejunal perforation after laparoscopic cholecystectomy, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw017, https://doi.org/10.1093/jscr/rjw017
Close - Share Icon Share
Abstract
Bowel perforation is a rare complication of laparoscopic cholecystectomy, which if left undiagnosed can have fatal consequences. In addition, isolated small bowel perforation is extremely rare and should be considered in patients presenting with sudden onset abdominal pain in the postoperative period. A 57-year-old male with symptomatic gallstones underwent urgent laparoscopic cholecystectomy and was discharged home on postoperative day (POD) 1 without complications. He presented to the emergency department on POD 11 complaining of sudden onset abdominal pain. A CT scan did not confirm a diagnosis and he was admitted for observation. On post admission day 2, he became significantly peritonitic and laparotomy revealed jejunal perforation. Bowel resection with hand-sewn anastomosis was completed and he was discharged on POD 10. Follow-up at 6 weeks revealed no further issues. We review the literature on small bowel perforation post laparoscopic cholecystectomy.
INTRODUCTION
Though rare, laparoscopic cholecystectomy is associated with electrothermal injury to the bowel, which may occur within or outside the laparoscopic field [1]. Such injuries can lead to fatal outcomes if a prompt diagnosis is not made at the time of presentation [1]. Electrothermal injury typically occurs by two mechanisms, direct contact by monopolar cautery with the tissue in question (contact injury) or by energy conduction through nearby tissue (conduction injury) [1]. Other authors also highlight the role of capacitive coupling [2, 3].
While there have been previous reports of electrothermal injury to large bowel, to our knowledge there have been no reports of such injury to small bowel resulting in perforation. We present the case of a patient who underwent laparoscopic cholecystectomy complicated by an apparent conduction burn injury of the small bowel presenting on postoperative day (POD) 11.
CASE REPORT
L.H. presented to the hospital complaining of sudden onset abdominal pain. He was nauseous and had one episode of emesis, but no prodromal symptoms. A past medical history was unremarkable. His only medication was aspirin 81 mg daily and his surgical history was significant for an uncomplicated laparoscopic cholecystectomy 11 days prior.
At presentation, his vitals were normal. Abdominal examination revealed an overweight gentleman with focal tenderness to the left upper quadrant. Laboratory tests revealed a WBC of 25.3 with neutrophils of 23.4. Hemoglobin, platelets, electrolytes and liver enzymes were within normal limits. Three views of the abdomen revealed no gross intra-abdominal pathology and no free air was reported on chest X-ray (Figs 1 and 2).

Chest X-ray showing left lower lobe opacity with a small volume of subdiaphragmatic free air.

A CT scan demonstrated significant soft tissue stranding/edema of the omentum in the left hemi-abdomen. In addition, there was mild ascites and multiple scattered locules of air (Figs 3–5). No other abnormality of the small or large bowel was identified. He was admitted for observation and broad-spectrum antibiotic therapy was initiated. On post admission day 2, he became diffusely peritonitic, febrile with a temperature of 39.1°C and his oxygen requirements increased to 12 l/min.
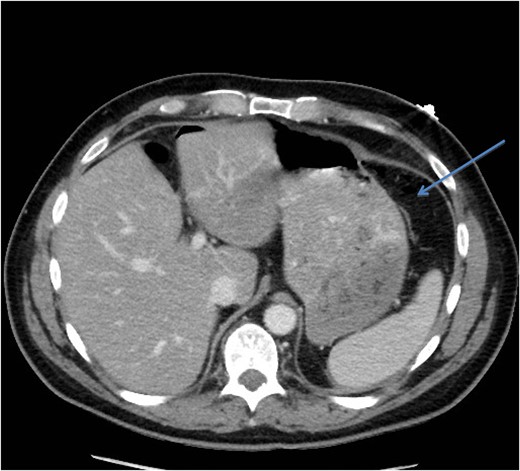
CT scan (axial image) demonstrating gas within the omentum (arrow).
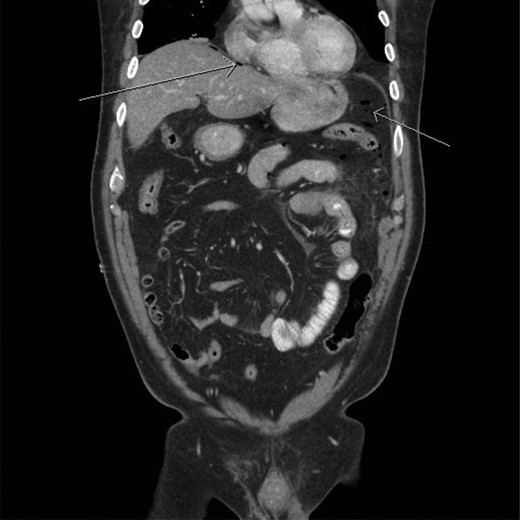
CT scan (frontal view) demonstrating multiple locules of air (arrows).

CT scan (frontal view) demonstrating stranding/edema to the omentum (arrow).
Exploratory laparotomy at this time interval revealed perforation of the jejunum with gross peritoneal contamination. After running the bowel, no other areas of compromise were noted. No evidence of soft tissue injury was seen and the omentum appeared intact. Resection and hand-sewn anastomoses were performed. The patient recovered well on the surgical service receiving 10 days of antibiotics. He developed an ileus postoperatively, which resolved with conservative management, and was discharged home on POD 10 with oral antibiotics. Histopathology revealed serositis with no focal ischemia or malignancy. Regular follow-up at 6 weeks revealed no further issues.
DISCUSSION
The overall complication rate for laparoscopic cholecystectomy is generally accepted at 3–7% [1], with the rate of bowel injury being 0.07–0.7% [1, 4]. Reports suggest that urgent procedures carry a significantly higher risk of postoperative complications, with rates between 7 and 18.5% [5–7]. Burn injuries in particular are rare, with an incidence rate of 0.07%, and are often not detected at the time of surgery, perhaps making this a lethal complication [1].
A literature search was conducted using the Medline, Ovid, EBSCO, PubMed and Google Scholar databases. Keywords included small bowel injury, laparoscopic cholecystectomy and laparoscopic surgery. Of 108 articles identified, only one case report described unanticipated thermal injury to the small bowel [8].
Our case demonstrates the diagnostic dilemma that accompanies delayed bowel injuries. Laboratory tests often give nonspecific results that seldom point to a diagnosis [1]. Imaging studies also fail to establish the etiology. Our CT scan failed to demonstrate significant intraperitoneal free air (Figs 3–5). In addition, oral contrast was utilized, but gross extravasation was not identified.
Polychronidis notes that given the likelihood of nonspecific test results, intestinal burn injuries must be included in the differential diagnosis of postoperative fever, persistent abdominal pain or general discomfort with signs of peritonism, even if they occur as late as 2 weeks from the time of surgery [1]. If symptoms are not relieved within a short period in hospital, an exploratory laparotomy should be performed [1]. Our patient's initial physical examination was deceptive, perhaps due to local control by the omentum.
Two features of our case that deviate from the typical picture of conduction burn injuries include the location of the injury as well as the lack of identifiable ischemia to the jejunal wall. Studies suggest that burn injuries typically occur at the duodenum and hepatic flexure due to proximity to the operative field [1, 9]. The mobility of the small bowel protects it from associated injuries as head-up/right-side up tilt allows the small bowel to fall away from the operative area.
The risk of conduction burn injury also decreases with increasing distance of structures from the operative field. This is because heat dissipates rapidly as it is conducted away from the site of primary contact due to the relatively high specific heat capacity of water [8]. The theoretical risk of conduction burn injury via the omentum itself still exists however. This risk is increased as monopolar diathermy is increased to high voltage settings, as is the case during hemostatic control [1, 2].
Burn injuries presenting in a delayed fashion are often secondary to delayed perforation at an ischemic site. Evidence of preceding ischemia is commonly seen at the time of surgery and is likely to be seen on microscopic analysis [1]. The lack of this finding in our case is unusual; however, missed trocar injuries typically present in the immediate postoperative period, further bolstering our etiology [10].
The risk of thermal injury to bowel during laparoscopic surgery should never be understated. Many authors advise against the use of monopolar cautery in this setting, and caution that if required, it should be used on the lowest setting possible to achieve adequate tissue dissection and hemostasis [1, 2, 9]. Ultrasonic energy devices are heralded as being safer in this regard, and some authors advocate their use in lieu of monopolar diathermy [9].
When morbidity occurs within the first 2 postoperative weeks, the differential diagnosis should include delayed perforation of any part of the bowel secondary to burn injury [1]. Perhaps, a safe approach is to presume that any patient presenting with worsening abdominal pain in this setting has a bowel injury until proven otherwise [1].
CONFLICT OF INTEREST STATEMENT
None declared.



