-
PDF
- Split View
-
Views
-
Cite
Cite
Yuyi Yeow, Yew-Lam Chong, Xanthogranulomatous pyelonephritis presenting as Proteus preperitoneal abscess, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw211, https://doi.org/10.1093/jscr/rjw211
Close - Share Icon Share
Abstract
Xanthogranulomatous pyelonephritis (XGPN) is a rare form of chronic pyelonephritis with progressive loss of renal function. Commonly, obstructing urinary calculi are seen. It is difficult to differentiate between XGPN and malignancy in many cases, and the diagnosis is usually only confirmed post-operatively upon histopathological examination of the specimen. Surgical treatment is often the main treatment modality due to suspicion for malignancy. Here, we present a case of XGPN that presented with abdominal distension, which was eventually discovered to be due to a preperitoneal abscess.
Introduction
Xanthogranulomatous pyelonephritis (XGPN) is an uncommon condition that can present in multiple ways. The index of suspicion should be present, especially in the setting of obstructive urolithiasis. Conservative treatment with antibiotics is an option in focal cases, but surgery is usually required in diffuse cases or when malignancy cannot be ruled out.
To the best of our knowledge, this is the first reported case of XGPN presenting with an anterior abdominal preperitoneal collection.
Case Report

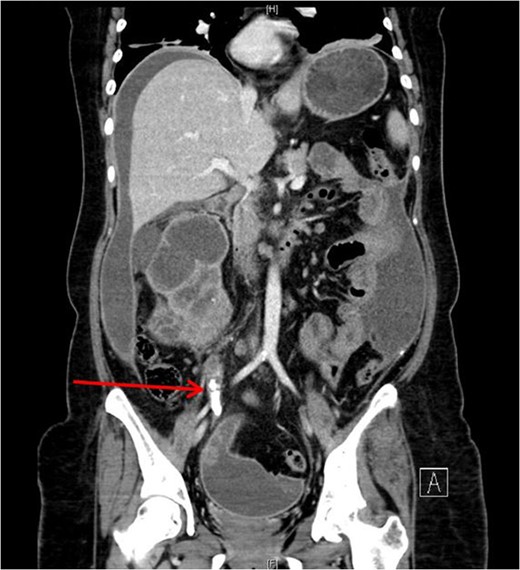
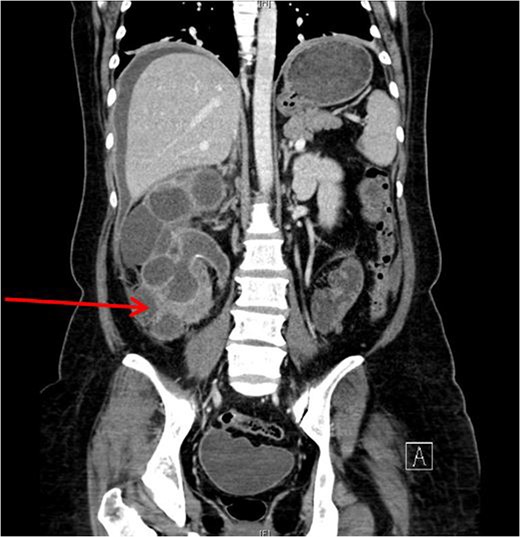
She underwent insertion of a right percutaneous nephrostomy drain, percutaneous drainage of the anterior abdominal collection, as well as a percutaneous biopsy of the right renal soft tissue lesion. Urine cultures from the percutaneous nephrostomy grew Proteus mirabilis. Fluid cytology from the abdominal collection showed acute inflammatory cells. Biopsy of the renal lesion showed xanthogranulomatous inflammation.
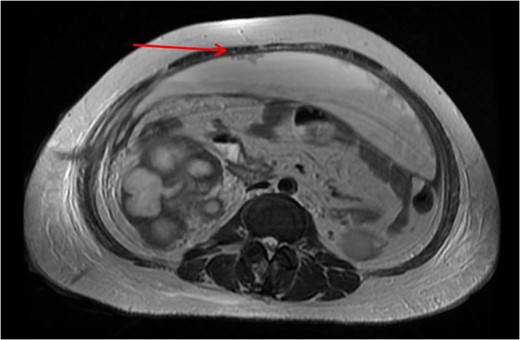
After a period of antibiotic treatment, she underwent open right nephroureterectomy with exploration, drainage and washout of the preperitoneal collection. During surgery, 1 l of pus was drained from the preperitoneal space, and cultures grew P. mirabilis. The ureter was ligated below the level of the calculus and removed together with the kidney. Final histopathology results showed XGPN with no evidence of malignancy in the kidney or peritoneal lining.
Post-operatively, she had small residual subhepatic collections, which were drained percutaneously, and she was discharged on the 11th post-operative day. She remained well on follow-up with no recurrence or complications.
Discussion
XGPN was first described in 1916 by Schlagenhaufer. Common associations are urinary tract obstruction, chronic urinary tract infections and urolithiasis. Other risk factors commonly seen are diabetes and hyperlipidemia.
A recently published case series of 12 XGPN [1] cases showed that only one patient presented with fever. Common presentations include a flank mass or flank pain. Other rare presentations described included septic lung metastasis [2] or fistulas.
Our patient had an atypical presentation with abdominal distension and presumed ascites, which was eventually revealed to be an anterior preperitoneal collection secondary to infection. Although the initial suspicion was that of a malignant process complicated by ascites, subsequent cytology and histopathological results showed that it was likely benign. In view of the non-functioning renal unit and significant abdominal collection, she underwent definitive surgery.
The most common urinary pathogen identified was Escherichiacoli [3], and common areas of involvement were the retroperitoneum and psoas muscle. In our patient, the retroperitoneal space was surprisingly not greatly involved, but rather it was the anterior preperitoneal space that had significant adhesions and inflammation. The pathogen identified from both nephrostomy and preperitoneal collection was P. mirabilis, showing that both pathologies were linked.
Previous authors have described laparoscopic approaches [4] for the treatment of XGPN, but this would unlikely have been suitable for our patient with a large anterior abdominal collection.
XGPN is also known as a great mimic, often indistinguishable from malignancy. Diffuse and focal forms have been described [5]. Conservative management with antibiotics [6], or partial nephrectomy [7], has been described for focal forms, but diffuse forms usually require total nephrectomy.
Conflict of interest statement
None of the contributing authors have any conflict of interest, including specific financial interests or relationships and affiliations relevant to the subject matter or materials discussed in the manuscript.



