-
PDF
- Split View
-
Views
-
Cite
Cite
Ali Kordzadeh, Bruno Lorenzi, Sritharan Kadirkamanathan, Alexandros Charalabopoulos, Laparoscopic transgastric removal of eroding gastric band: a different approach, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw207, https://doi.org/10.1093/jscr/rjw207
Close - Share Icon Share
Abstract
Gastric banding is a popular method for the treatment of morbid obesity. Amongst complications, gastric erosion remains uncommon but could prove fatal. Multiple techniques, from open surgery to endoscopic and standard laparoscopic technique for their removal, have been previously detailed in the literature. However, only a few reports have mentioned their total laparoscopic transgastric removal in the literature. Herein, we report a successful removal of an eroding gastric band with its technical suggestion in a 43-year-old female patient 22 months following its application.
INTRODUCTION
Laparoscopic adjustable gastric banding (LAGB) is an accepted and common procedure for morbid obesity. However, erosion of gastric wall is a recognized complication. In a systematic review by Egberts et al. [1], the overall incidence was 1.46% at mean follow up of 3.7 years. Upon detection of gastric band erosion, their immediate removal is highly advocated as their delay is associated with significant mortality and morbidity. Multiple techniques for band removal have been described. These include total endoscopic (endoluminal), laparoscopic, combined laparoscopic and endoscopic approach, and open surgery in complex cases. Amongst them, the endoluminal approach is the least invasive of all; however, this might not be feasible and applicable in some cases. When the anterior wall of the stomach is densely scared and there are some adhesions, and earlier techniques have failed to prevail, laparoscopic transgastric might be an effective technique if band cannot be safely removed [2]. Herein, we report a successful removal of an eroding adjustable gastric band with its technical suggestion in a 43-year-old female patient 22 months following its application.
CASE REPORT

Cross section CT image demonstration the site of the band with no collection (red arrow).
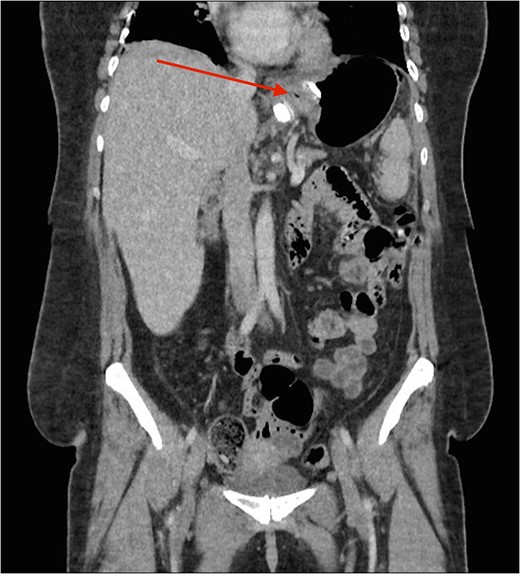
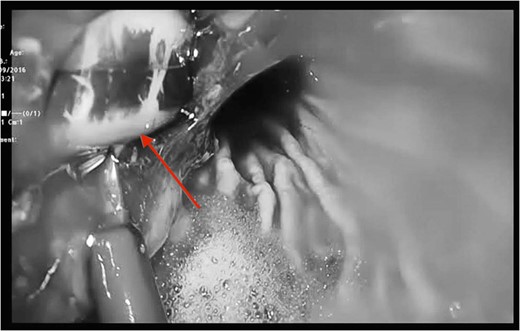
CT image demonstrating the air loculation site next to the band (red arrow).
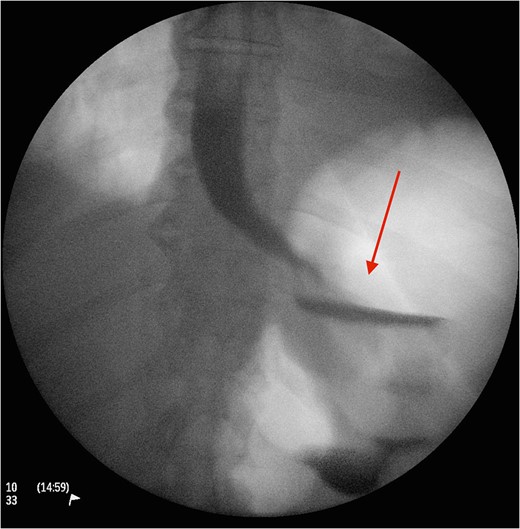
A postoperative Gastrografin swallow showing no leaks 3 days following the procedure.
DISCUSSION
Laparoscopic gastric banding remains an effective technique for the treatment of morbid obesity and is a primary and preferred choice for different centres. The reported complications vary from port site infection to band migration, pouch dilatation and gastric erosion. Amongst them, gastric wall erosion presents late (1–3 years) and the current reported incidence is estimated 0.3–14% [3]. Erosion can occur as a consequence of gastric wall ischaemia either secondary to a tight band and/or chronicity (pressure necrosis), peptic ulcer perforation, chronic inflammation due to contaminated device, binge eating and self-induced vomiting. In our reported case, patient did not suffer from any of the aforementioned factors apart from chronicity of the gastric band. The clinical presentation of gastric erosion is varied and but majority of individuals report abdominal pain, systematic inflammatory response (raised inflammatory markers) and in some advance cases perforation, sepsis and multi-organ failure [4].
The gold standard investigative modality is endoscopy [5]. CT is another option, although such tool is more useful in detection of associated complications such as extend, site and type of perforation and/or contaminations. Upon detection of erosion, removal remains the only option and should be performed promptly to avoid associated mortality and morbidity. The use of prophylactic antibiotics in such circumstance is not clear but in our centre we highly recommend their use upon suspicion of diagnosis. In case of band migration and/or erosion, endoscopic removal has shown promising results, although such technique is not always applicable and their open retrieval has been suggested and performed. Another option is standard laparoscopic division and retrieval. Although feasible and successful, this method does not always permit a comprehensive visualization, dissection and division. In our reported case, we encountered the aforementioned factors. Therefore, the decision was made to create anterior gastrotomies (extension of the port to stomach) to facilitate full division, retrieval of the gastric band and assessment of the erosion and its repair if necessary through transgastric approach. The authors believe, such procedure is safe and feasible in circumstances when standard laparoscopic retrieval is not possible. Placement of a new gastric band is usually delayed for a period of 3 months in such cases [3, 5]. In the reported case, patient made an uneventful recovery and was discharged 3 days following the procedure.
In conclusion, transgastric division and removal of gastric band is safe, feasible and a good alternative when standard approach is not feasible. This procedure is associated with short recovery period and early discharge. Written informed consent was obtained from the patient for publication of this case report and accompanying images. No identification details have been used.
CONFLICT OF INTEREST STATEMENT
None declared.



