-
PDF
- Split View
-
Views
-
Cite
Cite
Moosa Kunhi, Sachin Sanagar, N Jagadeesh, Bhima Shankar, Abi Abraham, Emergency cardiac double valve surgery in active infective endocarditis due to Acinetobacter baumannii with aortic root abscess in a patient with dialysis-dependent end-stage renal failure: a rare case report, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw168, https://doi.org/10.1093/jscr/rjw168
Close - Share Icon Share
Abstract
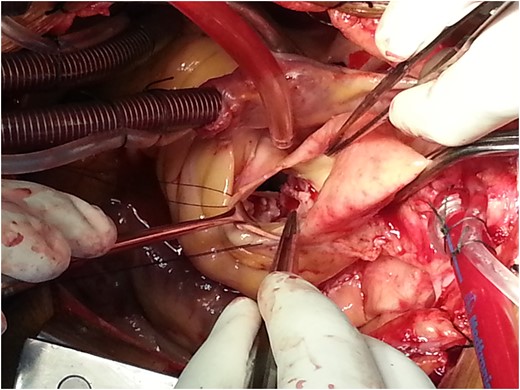
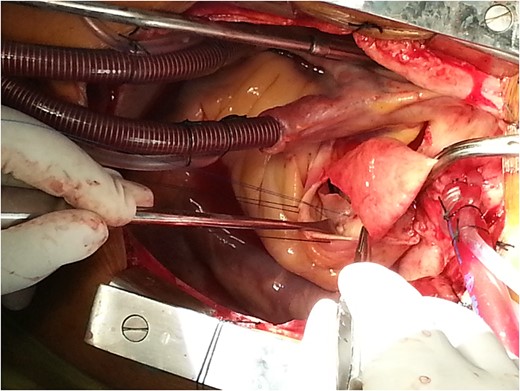
We report an end-stage renal disease (ESRD) patient on regular haemodialysis awaiting renal transplant having native aortic valve endocarditis due to Acinetobacter baumannii complicated with aortic root abscess and severe mitral valve regurgitation with NYHA class IV symptoms. He underwent emergency aortic root abscess debridement, reconstruction with autologous pericardial patch and bioprosthetic aortic valve replacement along with mitral valve repair. This emergency intervention in active infective endocarditis due to A. baumannii and associated ESRD is very rare. We could not trace any case report for such combination of clinical scenario in the literature.
INTRODUCTION
The literature is limited on outcomes of valvular replacement surgery in dialysis-dependent end-stage renal disease (ESRD) patients with active bacterial endocarditis [1]. Aortic root abscess is a complication of aortic valve infective endocarditis having high morbidity and mortality. Infective endocarditis due to Acinetobacter baumannii is very rare. Early diagnosis and prompt surgical intervention is must to save the life of a patient. We operated a 39-year-old patient having severe aortic regurgitation, severe mitral regurgitation, active bacterial endocarditis and aortic root abscess due to A. baumannii with dialysis-dependent ESRD.
CASE REPORT
A 39-year-old non-hypertensive non-diabetic male patient, a bank manager by profession, was admitted in our hospital with ESRD having high-grade fever. He was on regular haemodialysis for the last 1 year. He had a history of cerebrovascular accident and full recovery 8 weeks prior to this admission. His symptoms deteriorated from NYHA class II to IV in a short span of 2 weeks.
On clinical examination, the patient looked pale with a pulse rate of 90/min regular collapsing in nature. Blood pressure was 96/48 mmHg. Grade 2 clubbing was present along with bilateral pedal oedema. There were no icterus, cyanosis or lymphadenopathy. Cardiac examination revealed raised JVP with cardiomegaly. Third heart sound (S3) was audible along with a soft blowing early diastolic murmur in the third left intercostal space and radiating along the left sternal border with systolic flow murmur in the aortic area.

DISCUSSION
Emergency Double Valve Surgery in active infective endocarditis with aortic root abscess in a patient with dialysis-dependent ESRD is extremely rare. Data are scarce.
In one major study, in-hospital mortality of dialysis patients undergoing valve surgery is reported to be 20.7% [2]. Thirty-day mortality for aortic root abscess surgery is 20–25% [3]. In our case, we had a combination of above conditions, dialysis-dependent ESRD and aortic root abscess making it a very high risk surgery. Also surgery on emergency basis increased the risk manifold. We could not find exact reported mortality as such combination is rare in the literature. We found one such case in a similar patient as an emergency case has been reported [4].
These ESRD patients are usually anaemic, commonly have platelet dysfunction and are prone to have postoperative bleeding. Postoperatively, electrolyte and volume management in these patients can be problematic, and risks of pulmonary, cardiac and neurological complications are high.
Endocarditis affecting the aortic valve leading to abscess formation is particularly challenging to treat and requires aggressive diagnostic and therapeutic approaches because of severe complications such as conduction block, destruction of surrounding tissue, fistula to other cardiac chambers, aortic pseudoaneurysm formation and extrinsic compression of coronary arteries [5]. The most important aspect in the surgical treatment of these patients is radical debridement of all infected tissues. Reconstruction with pericardial patch and valve replacement with either aortic prosthetic valve or homograft is done. In our case, bioprosthetic valves were used because homografts were not available in emergent situations, and the cost of a homograft is also too expensive to procure it on emergency basis. Due to the limitation of related articles of similar clinical scenario of aortic root abscess due to A. baumannii in dialysis-dependent patient along with intervention for two cardiac valves, there was no possibility of further survey and comparison.
Acinetobacter baumannii is very rare to cause infective endocarditis. The first case of infective endocarditis by A. baumannii in a haemodialysis patient from China was reported in 2012 [6].
In conclusion, one should not deter going ahead with emergency surgery for aortic root abscess in active infective endocarditis in dialysis-dependent renal failure patients even though it is a grave clinical situation with high morbidity and mortality. Clinical literature is very scarce. The rarity in the literature of such clinical scenario makes our case report very unique.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- pericardial sac
- mitral valve insufficiency
- hemodialysis
- mitral valve repair
- bacterial endocarditis
- renal transplantation
- kidney failure, chronic
- debridement
- abscess
- reconstructive surgical procedures
- heart
- acinetobacter baumannii
- new york heart association classification
- heart valve surgery
- supraaortic valve area
- aortic valve endocarditis
- bioprosthetic aortic valve replacement



