-
PDF
- Split View
-
Views
-
Cite
Cite
Atsushi Suga, Shunsuke Yamada, Haruka Takeichi, Yusuke Nakamura, Masayuki Iwazaki, L-shaped mini-sternotomy combined with videoscopic approach for thymoma with invasion of major veins, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw199, https://doi.org/10.1093/jscr/rjw199
Close - Share Icon Share
Abstract
It might be possible to remove thymic tumors with minimal invasion of the left brachiocephalic vein (BCV) using an advanced videoscopic technique; simple resection of this vessel can be achieved via such an approach. However, tumor invasion of the superior vena cava or right BCV requires angioplasty or reconstruction, both of which are difficult to perform in videoscopic procedures. We report a case of invasive thymoma with localized invasion of the great vessels at the junction of the left BCV and superior vena cava. An L-shaped mini-sternotomy combined with a videoscopic approach allowed thymectomy with safe vesselplasty of the involved vessels.
Introduction
We report a case of invasive thymoma with localized invasion of great vessels at the junction of the left brachiocephalic vein (BCV) and superior vena cava. An L-shaped mini-sternotomy combined with video-assisted thoracic surgery (VATS) allowed thymectomy with safe vesselplasty of the left innominate vein.
Case
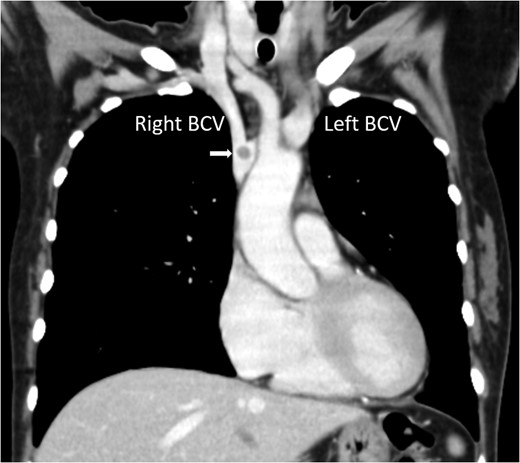
Chest computed tomography showing a nodule at the junction of the right and left BCV (arrow).
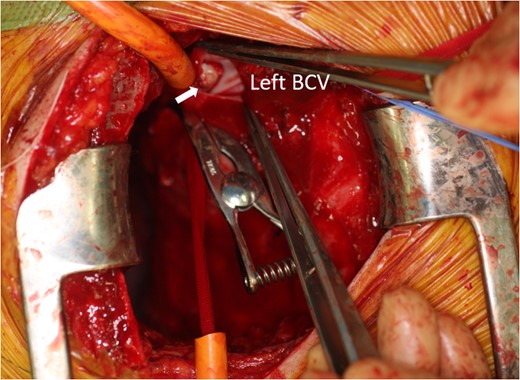
Intraoperative photo showing the tumor extending into the left BCV (arrow).
Discussion
It is commonly believed that only non-invasive thymomas within 5 cm in diameter can be managed by VATS. However, recent advances in videoscopic techniques have allowed resection of localized thymomas invading the lungs, phrenic nerve and pericardium [2]. Because simple resection of the left BCV is possible, VATS can be performed in cases with minimal invasion of this vessel. On the other hand, when tumor invasion has occurred at the level of the right BCV or SVC, angioplasty or vessel construction is required. These procedures are difficult to perform in videoscopic procedures but can be achieved by the addition of minimally invasive surgery, thus minimizing the incidence of sternal dehiscence and infections, which occur in 0.5–5% of open heart surgeries [3]. The risk of sternal complications was likely greater in the present case because she was receiving high-dose steroid therapy. Sternal instability would have caused serious respiratory complications in this patient, who may again have developed an MG crisis. We, therefore, aimed to minimize surgical damage to the thorax. A combined mini-sternotomy/VATS technique for performing thymectomies in patients with MG and minimally invasive treatment of cardiovascular disease has been reported [4, 5]. In our case, an L-shaped sternotomy provided sufficient surgical exposure of major veins and allowed accurate angioplasty of these vessels. If the surgical field is inadequate for this procedure, then conversion to a reversed T or full sternotomy is easily achieved [5]. Adding mini-sternotomy to VATS can facilitate angioplastic procedures on major vessels.
Conflict of interest statement
None declared.



