-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Ching, Giles Davies, Primary ectopic breast carcinoma of the axilla in a male patient, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw193, https://doi.org/10.1093/jscr/rjw193
Close - Share Icon Share
Abstract
Primary ectopic breast carcinoma in male is very rare. We report a case on a 52-year-old gentleman who presented initially with bilateral lesions in his axilla and after delayed diagnosis the right lesion was confirmed as an ectopic breast carcinoma. We reviewed the literature and discussed the significance of the case.
INTRODUCTION
CASE
A previously fit and well 52-year-old Caucasian gentleman presented to his general practitioner (GP) with bilateral skin lesions in his axilla that had been present for the last 2 years. He had a positive family history of BC, with two paternal aunts and a cousin affected. Examination revealed an area of suspected keratosis located in the left axilla, with a probable pigmented nevus in the right axilla. Both were felt to be benign and patient was reassured. The patient re-presented 6 months later complaining of discomfort from the lesion in the right axilla. On second examination, the nodule had increased in size from 0.5 to 1.5 cm in diameter, and was becoming marginally red and prominent.
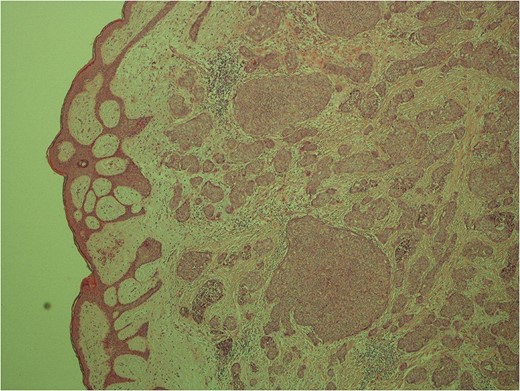
Low power image demonstrating the skin surface and dermal nests of tumour completely filling the tissue.
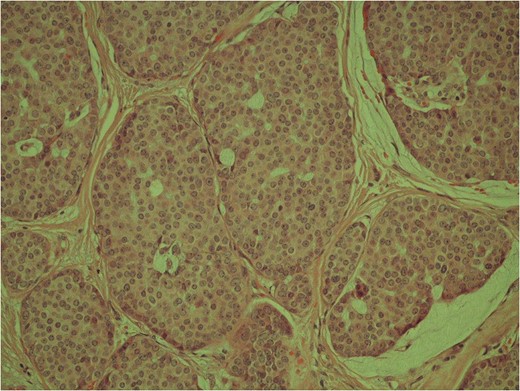
High power image of the dermal nests of tumour showing solid islands of invasive breast carcinoma.
The case was discussed at the multidisciplinary team. Taking into account the clinicopathological correlations, the tumour was diagnosed as a PEBC. A re-excision of the right axillary scar with a sentinel lymph node biopsy and a wide local excision of the left axillary nodule were performed. Final histology of the right re-excision revealed no residual malignancy or any nodal involvement. The lesion from the left axilla was confirmed as a seborrheic keratosis. No adjuvant radiotherapy or chemotherapy was recommended. The patient completed treatment with Tamoxifen 20 mg once daily for 5 years. Follow-up 5 years post-diagnosis confirms patient remains disease-free.
DISCUSSION
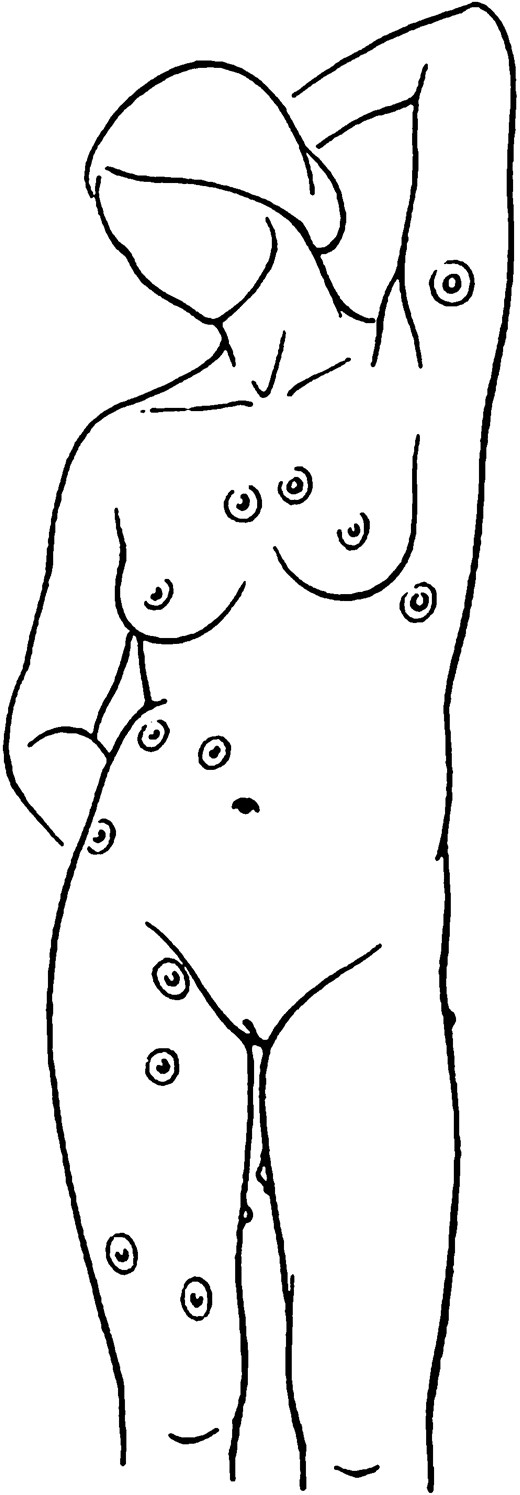
PEBC sites are not routinely screened and they remain unnoticed until clinical features develop. The most commonly reported clinical feature is the presence of a palpable mass [4]. Swelling, erythema, pain and discomfort are less often observed. It has been postulated that risk factors for BC may also apply for ectopic tissue. As demonstrated in our case, our patient did have familial predisposition to BC.
Suspicious mass around the axilla can be the result of several aetiologies including benign or malignant lymphadenopathy, lymphoma or metastatic carcinoma. The two most common histological diagnoses is invasive ductal carcinoma (40–70%), followed by invasive lobular carcinoma (12%), which is similar in eutopic BC [3]. Histological diagnosis can occasionally be challenging. In our case, the presence of malignant cells in the excised nodule with normal surrounding breast tissue that was ER and PR positive confirmed the diagnosis.
To date, there are only six cases of PEBC reported in males [3]. Due to its rarity and low index of suspicion especially in males, it is often not on the differential diagnoses list which leads to delayed diagnosis. There are currently no guidelines on diagnosis and/or management of PEBC. The management approaches reported in the literature are based on BC treatment guidelines. Ipsilateral prophylactic mastectomy confers no additional benefit and is unnecessary [5]. In all cases, the contralateral breast and axilla should also undergo full investigation. It is worth noting that PEBC can occur in various parts of the body and may require further investigation on the lymphatic drainage with an individualized management plan.
The prognosis of PEBC is contentious; some consider it similar to BC but others argue that it has worst prognosis due to higher chance of lymph node involvement [6, 7]. The difficulty in diagnosis contributing to the rare incidence and lack of reporting in literature precludes detail evaluation of the management and prognosis.
We have reported a rare case of PEBC of the axilla in a male patient. In the presence of an enlarged axillary nodule, the possibility of PEBC should always be considered by the clinician even in male patients. Further research is required to establish best practice.
conflict of interest statement
None declared.



