-
PDF
- Split View
-
Views
-
Cite
Cite
Keith Pace, Karl Spiteri, Karl German, Spontaneous proximal ureteric rupture secondary to ureterolithiasis, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw192, https://doi.org/10.1093/jscr/rjw192
Close - Share Icon Share
Abstract
We present the case of a 37-year-old lady who presented with severe colicky left sided flank pain associated with vomiting, chills and rigors. A non-contrast Computed Tomography of the Kidney Ureter and Bladder was performed which showed a 2–3 mm stone in the pelvic part of the left ureter. Following 2 days of conservative treatment she was still complaining of increasingly severe pain. A contrast computed tomography of the abdomen was performed which was suggestive of a perforation of the left collecting system. A diagnosis of spontaneous left proximal ureteric perforation secondary to urolithiasis was made. We opted to treat her with retrograde endoscopic ureteric stent insertion. Spontaneous rupture of the ureter is a relatively rare urological occurrence with only a small number of cases reported in the literature. Although there are no recommendations, ureteric double-J stenting is the most commonly used management option with good results reported.
INTRODUCTION
Spontaneous rupture of the ureter is a rare urological occurence with only a small number of cases reported in the literature. It is defined as extravasation of urine from the ureter which occurs without trauma or iatrogenic manipulation of the ureter. It often occurs secondary to uretrolithiasis with urinary tract obstruction and resultant increased intraluminal pressure and subsequent rupture [1]. It may also be secondary to a tear of the ureter during passage of the stone [2]. Peritoneal irritation by urine results in presentation with an acute abdomen, sometimes without any urinary tract symptoms or urinalysis abnormalities. Owing to its presentation it is often misdiagnosed as appendicitis or diverticulitis [3].
Reported patients have an average age of 42 years, with no sex predominance [4].
Rupture may occur anywhere along the urinary tract, with the commonest sites being the fornices and upper ureter. It may lead to urinoma, infection with sepsis, acute kidney injury and abscess formation if left untreated [1].
CASE REPORT
A 37-year-old previously healthy lady, presented at the accident and emergency department complaining of severe colicky left sided flank pain associated with two episodes of vomiting and chills and rigors. She denied any associated dysuria, haematuria or frequency.
On examination she was found to be tender in the left flank with a positive renal punch. Her abdomen was non-peritonitic and she was haemodynamically stable and afebrile. She was given analgesia with little effect.
A non-contrast CT KUB was performed which showed a 2–3 mm stone in pelvic part of the left ureter.
Despite the very small stone size and distal position in the ureter making her a good candidate for conservative treatment, she was admitted to the urology department for further care due to her unremitting severe pain. She was prescribed intravenous Hartmann's solution at 125 ml/hr and given appropriate analgesia. She was also advised to start oral Tamsulosin as part of metabolic expulsive therapy, but she refused this as it is only licensed for use in men for treatment of lower urinary tract symptoms secondary to benign prostatic hypertrophy.

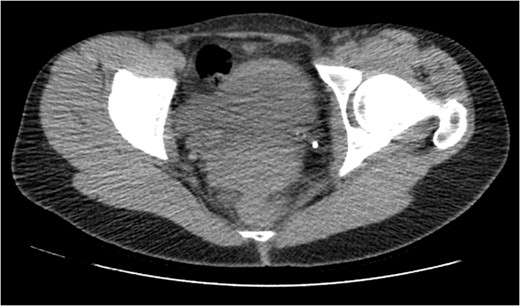
CT IVU- confirmed extravasation of contrast medium around the left kidney and ureter, the rupture being at the level of the PUJ.

Coronal view reconstructions using maximum intensity projection, showing proximal ureteric leak of contrast.
Blood tests, clinical parameters and temperature were still well within normal limits, despite the severity of symptoms and clinical examination. We opted to treat her with retrograde endoscopic ureteric stent insertion. A 6-French long-term stent was inserted uneventfully across the defect. A 16 F urethral catheter was inserted to avoid reflux. The patient was also started on intravenous ciprofloxacin and piperacillin/tazobactam post operatively.
On Day 9 since presentation a CT IVU was repeated. This showed the stent in the left ureter to be in situ with no further leakage from the known rupture.
On Day 10 the patient underwent a successful trial without urinary catheter and was discharged home with an appointment for removal of stent and retrograde pyelography in 3 months.

On table Pyelogram confirmed intact left collecting system and ureter.
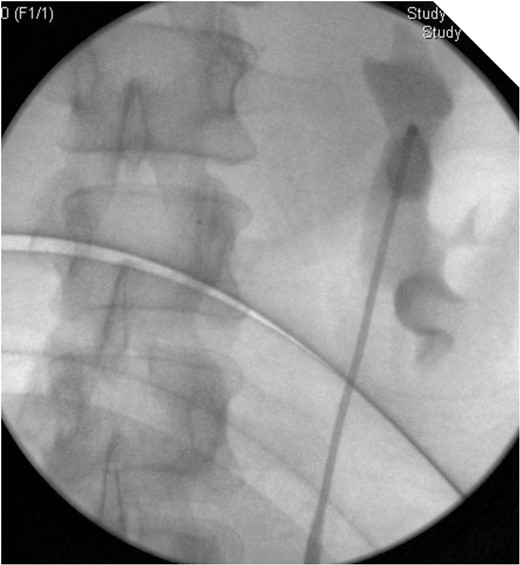
On table Pyelogram confirmed intact left collecting system and ureter.
DISCUSSION
Spontaneous ureteral rupture is a surprisingly rare condition. It is by definition non-traumatic in origin, and can be difficult to diagnose unless a high index of suspicion for this condition is maintained. The most common cause for spontaneous ureteral rupture are obstructing ureteral calculi. Other reported rarer causes include tumour, retroperitoneal fibrosis, pregnancy, connective tissue disorder and acute urinary retention.
The condition should be suspected in cases of ureteric colic which develop significant acute worsening of symptoms [1], with increased areas of tenderness, with or without a reactive peritonitis. Imaging is required to confirm the diagnosis. Whilst ultrasound can be helpful in identifying a perinephric or retroperitoneal fluid collection, the condition is best diagnosed with a delayed CT scan post-intravenous contrast. This modality will confirm a urinary leak and can accurately define the site of rupture [5, 6]. Coronal reconstructions may further help in accurately identifying the site of leak. The use of a delayed film post IV contrast is also very useful in differentiating a ureteral rupture from an infective perinephric abscess that can also arise from obstructing calculi. It can also differentiate from forniceal rupture.
Due to the rarity of this clinical condition, there are no guidelines or recommendation on its’ management. We managed our patient with retrograde insertion of a double-J ureteral stent which was then removed after 12 weeks. On reviewing case reports of patients with this condition, the majority were also managed with a double-J ureteral stent. Conservative management was adopted in a smaller amount of patients [7]. Percutaneous drainage with or without nephrostomy/antegrade stent is another reported option [8, 9].
Development of fever or haemodynamic changes may indicate an infective process of the resulting urinoma and antimicrobial therapy ± drainage needs to be considered. A high serum creatinine may also be noted from reabsorbtion of the urinoma.
On stent removal, we performed an on table retrograde pyelogram to confirm there is no residual leakage and also to exclude significant stricturing. A CT IVU after stent removal may also be considered as an alternative to this approach.



