-
PDF
- Split View
-
Views
-
Cite
Cite
Nisha Pindoria, Yurina Miki, Andrea Tay, Ashish Chandra, Christopher Anderson, Evangelos Zacharakis, Majed Shabbir, Epididymal papillary cystadenocarcinoma metastasising to the testis in a patient with infertility managed with Onco-microTeSE, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw191, https://doi.org/10.1093/jscr/rjw191
Close - Share Icon Share
Abstract
Papillary cystadenomas of the epididymis are known to occur in association with Von Hippel–Lindau (VHL) disease. The development of a papillary cystadenocarcinoma, its malignant counterpart, is rare with only a few sporadic cases reported in the literature. Metastatic deposits are exceedingly uncommon; in fact, only a single case report has documented metastases to the paraureteral region, but metastases to the testis have never been reported. A 43-year-old gentleman with VHL disease presented with non-obstructive azoospermia, a right epididymal mass, and an atrophic surgically corrected undescended left testis. The epididymal mass was reported as a papillary cystadenocarcinoma on biopsy. The patient was managed with a radical inguinal orchidectomy and bench microTeSE with successful sperm retrieval. Metastatic papillary cystadenocarcinoma of the epididymis to the testis has never been previously reported. This case was managed by radical orchidectomy and subsequent onco-microTeSE, allowing safe oncological treatment and optimal fertility preservation.
INTRODUCTION
Von Hippel–Lindau (VHL) disease is a rare inherited condition affecting 1 in 36 000 births and is associated with the development of various multi-system tumours, including haemangioblastomas, phaeochromocytomas, renal cell carcinomas, endolymphatic sac tumours and papillary cystadenomas of the epididymis (in men) and broad uterine ligament (in women) [1]. Although the association between VHL and primary epididymal papillary cystadenomas is well known, there is extremely limited information about its malignant counterpart (i.e. papillary cystadenocarcinomas) with only a few cases reported in the literature [2–6]. The few case reports available have not been associated with VHL disease. As a result, there is also limited information regarding their optimal long-term management.
We present the first reported case of a 43-year-old gentleman with VHL disease presenting with azoospermia and subsequently diagnosed with a primary epididymal papillary cystadenocarcinoma, infiltrating the spermatic cord and accompanied by a metastatic deposit in the right testis. The patient was ultimately managed by a combination of radical orchidectomy and onco-microTeSE.
CASE REPORT
A 43-year-old gentleman with known VHL disease and a history of multiple renal carcinomas presented with primary infertility and non-obstructive azoospermia. On examination, he had an atrophic left testis (secondary to a previous orchidopexy for cryptorchidism) and a firm mass in the right epididymis. He was referred for testicular sperm extraction. At the time of surgical sperm retrieval, a biopsy was taken from the epididymal mass, which was reported as a cystadenocarcinoma. A further biopsy was taken of a mass incidentally noted in the upper pole of the right testis, which on histology was suggestive of a metastatic deposit of renal cell carcinoma. No other sites of renal metastasis were seen on subsequent imaging. An orchidectomy was advised, but declined by the patient as he was keen to start a family.
After successfully having a child via in vitro fertilisation (IVF) treatment, he re-attended the urology department for definitive management of his epididymal and testicular tumours. He was asymptomatic and clinical examination revealed a palpable mass in the head of the epididymis measuring ~1.5 cm. A separate small mass was also palpable in the upper pole of the right testis. Blood tests revealed normal testicular tumour markers (α-fetoprotein, β-human chorionic gonadotrophin and lactate dehydrogenase). Follicle stimulating hormone and leutenizing hormone levels were 36 and 13 mIU/mL respectively, with a testosterone level of 12.2 nmol/L.
Preoperatively, the optimal management strategy of his testicular and paratesticular lesions was complicated given the rarity of the case coupled with the challenge of multiple issues including:
Future fertility preservation.
Atrophic, previously undescended, contralateral testis.
Borderline testosterone levels.
Propensity to develop further tumours on a background of VHL disease.
Initially, a partial orchidectomy was considered to preserve future fertility. However, after review at the multidisciplinary team (MDT) meeting, it was felt that a radical orchidectomy was the safest oncologocial management option and was agreed by the patient. This was performed via an inguinal approach and an onco-microTeSE (microsurgical testicular sperm extraction in azoospermic cancer patients performed once the testicle has been removed) was carried out to allow for future family planning. Isolated areas of dilated tubules were retrieved under ×20 magnification with viable sperm cryopreserved for future IVF. Post-operatively, there were no reported complications.
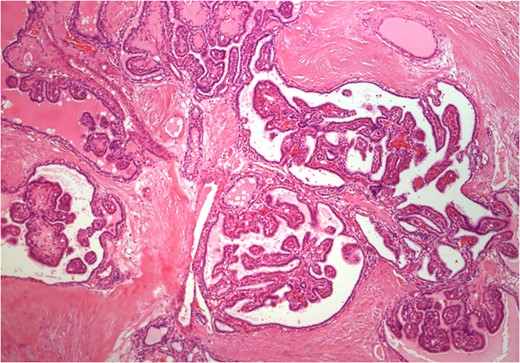
Histology of epididymal tumour showing varying architectural patterns. In some areas, the epididymal tumour resembled that of a classical papillary cystadenoma (4× magnification).
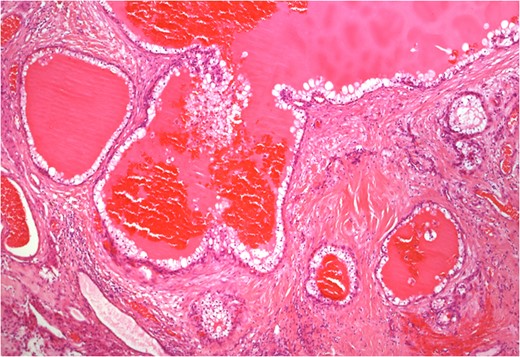
Histology of separate tumour deposit in testis composed of cystic spaces filled with eosinophilic secretions and lined by polygonal cells with clear cytoplasm (4× magnification).
Given the unusual nature of the case, the unknown prognosis of papillary cystadenocarcinomas and the lack of established treatment protocols post-orchidectomy, an MDT decision of close clinical surveillance with regular follow-up was made.
DISCUSSION
This case is interesting on a number of levels. Papillary cystadenomas of the epididymis are known to occur in association with VHL disease. However, the development of a papillary cystadenocarcinoma, its malignant counterpart, is incredibly rare. There is a single case report, which has documented metastases from such tumours to the paraureteral region [7]. However, metastasis to the testis has not been previously reported in the available published literature. The presentation on a background of infertility and atrophic undescended contralateral testis raises further dilemmas in management.
Surgical debulking remains as the cornerstone for the treatment of primary malignant epididymal tumours either via partial or radical orchidectomy. A radical orchidectomy was considered to be the optimal treatment in view of the nature and location of his tumour, but the limited functional potential of his contralateral atrophic testis made his management more challenging. In this case, fertility preservation was paramount to the patient. Combining his radical orchidectomy with a simultaneous surgical sperm retrieval using an onco-microTeSE allowed safe oncological management and optimal fertility preservation. Referral to specialist units with expertise in performing onco-microTESE is important in such difficult cases.
CONSENT
Written consent was obtained from the patient for publication of this case report and the accompanying images.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared.



