-
PDF
- Split View
-
Views
-
Cite
Cite
Angus Hann, Edoardo Osenda, Jon A. Reade, Demetrius Economides, Dinesh Sharma, Case report: successful open resection of a symptomatic giant liver haemangioma during the second trimester of pregnancy, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw185, https://doi.org/10.1093/jscr/rjw185
Close - Share Icon Share
Abstract
Liver haemangiomas are consistently reported to be the commonest benign liver tumours and are most often incidental findings in asymptomatic individuals. Large lesions can become symptomatic, spontaneously rupture or result in a consumptive coagulopathy known as Kasabach–Merrit Syndrome. It is believed that the female sex hormones, particularly oestrogen, have an influence on haemangioma development and growth. The optimal management of large haemangiomas during the hyperoestrogenic state of pregnancy is poorly described in the current literature. To our knowledge, we describe only the second case of a giant hepatic haemangioma resection during pregnancy.
INTRODUCTION
Haemangiomas are the most common benign liver neoplasm and result from ectatic growth of the vasculature [1]. These lesions can grow to a significant size and are referred to as giant haemangiomas once larger than 5 cm. Despite the absence of invasive or metastatic potential, hepatic haemangiomas can result in pain, obstructive symptoms, rupture with life threatening haemoperitoneum or a consumptive coagulopathy known as Kasabach–Merrit syndrome [2]. Consensus agreement on the indications for surgical resection, other than for symptomatic lesions, including for giant haemangioma, is lacking at present [1]. There is a paucity of available literature outlining the behaviour of haemangiomas during pregnancy, however female sex hormones have been implicated in their pathogenesis and growth [3]. The nature and extent of this relationship is yet to be fully elucidated. On the other hand, the diagnosis of a symptomatic giant haemangioma during pregnancy presents a dilemma because the safety of neither conservative nor surgical resection has been rigorously investigated. At our centre, a 30-year-old G2P0M1 female underwent resection of a symptomatic giant hepatic haemangioma during the second trimester without any complication.
CASE REPORT

Coronal CT image in the portal venous phase demonstrating the large exophytic haemangioma.

Axial CT image in portal venou phase at level slightly inferior to aortic bifurcation demonstrating the peripheral nodular enhancement of the haemangioma.
On first review in our clinic the patient was 6 weeks pregnant. She was counselled by a consultant liver surgeon and obstetrician about the available management options and associated risks. The surgical options discussed included; close observation throughout pregnancy and elective resection post-partum, termination of pregnancy followed by resection or resection during the second trimester of pregnancy. Our patient decided to have the tumour resected whilst pregnant due to the concern of rupture, accepting the risks of surgery to herself and the foetus. The operation was scheduled for the second trimester as this is the period in which subsequent miscarriage or preterm labour are least likely [5].
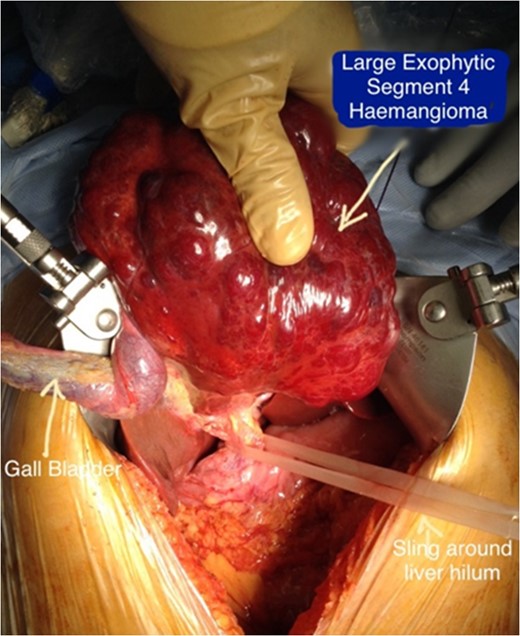
Intraoperative image demonstrating the exophytic nature of the haemangioma and relevant anatomical structures.
Obstetric examination in the immediate post-operative period was consistent with a healthy foetus and the patient was discharged from hospital on the third post-operative day. Histopathological examination of the tumour confirmed a haemangioma weighing 412 g. The patient received outpatient follow-up and did not experience any surgical or obstetric complications. A healthy infant was delivered at term via an elective caesarean section due to maternal request.
DISCUSSION
There is little available literature describing the outcome of liver haemangioma resection during pregnancy. To our knowledge, the only available publication is an isolated case report of a successfully resected giant haemangioma at 16 weeks gestation due to Kasabach–Merit Syndrome [6]. The scarcity of data may be representative of how infrequently this operation is performed during pregnancy. Both pregnancy and hormonal therapy, including the oral contraceptive, have been associated with haemangiomas enlargement [3]. Descriptions of tumour growth and complications during pregnancy are conflicting. Rapid growth [7] and haemorrhagic complications [8] have been reported but a recent small case series (four patients, seven pregnancies) found that these tumours can be safely observed during pregnancy [2]. A larger observational cohort study in non-pregnant individuals found that haemangioma resection can be justified due to minimal morbidity and no mortality in the 13 patients who underwent surgery [9]. However, these authors also found that no tumours under 5 cm increased in size or ruptured in patients who received conservative management. Obviously, extrapolation of these findings to our patient would be misguided as the large peripheral exophytic tumour was >5 cm and she was pregnant.
Spontaneous rupture is the complication most feared because this is associated with a mortality rate approaching 80% [6]. A recent large study has estimated that the rupture rate of giant liver haemangioma is 3.4% with peripherally located and exophytic lesions being at higher risk [10]. Accelerated growth, increased intra-abdominal pressure and direct contact with the gravid uterus are all plausible mechanisms for spontaneous rupture or worsening symptoms during pregnancy. Intrapartum rupture of liver haemangiomas has been reported, supporting the notion that increased intra-abdominal pressure may be a causative factor. Our patient's tumour was assessed as being high risk for complications during pregnancy due to its size, exophytic nature and subumbilical position. Therefore, we felt that the risks associated with surgery were justified in this case as spontaneous or intrapartum rupture could be an unsurvivable event.
To our knowledge, this is only the second case report of a successful hepatic haemangioma resection during pregnancy. The natural history of these lesions during pregnancy is incompletely understood and resection should be considered if worsening symptoms or the clinical concern for rupture is significant. An interdisciplinary approach that involves surgical, anaesthetic and obstetric specialists is required to perform this procedure safely, and a good overall result for mother and child is possible.
CONFLICTS OF INTEREST STATEMENT
None to declare.



