-
PDF
- Split View
-
Views
-
Cite
Cite
Zoheb Berry Williams, Nicole M. Organ, Stephen Deane, Inferior vena caval filter strut perforation causing intramural duodenal haematoma, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw170, https://doi.org/10.1093/jscr/rjw170
Close - Share Icon Share
Abstract
We present a case of intramural duodenal haematoma caused by inferior vena caval (IVC) filter strut perforation requiring innovative open and endovascular retrieval. A 32-year-old woman presents in shock with dull epigastric pain and non-bilious vomiting. She had previously had an IVC filter for deep venous thrombosis and pulmonary embolism. Computed tomography demonstrated strut perforation into the second part of the duodenum, causing intramural haematoma and duodenal obstruction. Laparotomy facilitated evacuation of the duodenal haematoma, while the IVC filter was retrieved by endovascular means. Causes of duodenal haematoma include blunt trauma, haematologic malignancy, coagulopathy, percutaneous or endoscopic procedures, pancreatic pathology, peptic ulcer disease and aortoenteric fistula. Duodenal haematoma is rare and is usually managed conservatively or by percutaneous drainage. While this patient had a typical presentation, IVC filter strut perforation has not been described in the literature as a cause for duodenal haematoma.
Introduction
Duodenal haematoma rare. It is often caused by blunt trauma, haematologic malignancy, coagulopathy and percutaneous or endoscopic procedure. It is also usually suitable for conservative management or percutaneous drainage. We present a case of intramural duodenal haematoma caused by inferior vena caval (IVC) filter strut perforation managed by laparotomy and endovascular filter retrieval. This cause of duodenal haematoma is not repeated in the world literature to our knowledge.
Presentation of Case
A 32-year-old woman presented with a 24-hour history of constant dull epigastric pain, nausea and non-bilious vomiting. This was her second similar presentation to the emergency department within 24 hours. She denied any abdominal trauma. Her background was significant for Bechet's disease and Takayasu's arteritis, which required immunosuppression with mycophenolate and prednisone, peptic ulcer disease, aortic valve replacement, hypertension, aorto-iliac bypass with visceral and renal revascularization for severe chronic visceral and lower limb ischaemia 12 months ago, she had an infrarenal IVC filter (Celect, COOK) placed at that time because of a history of deep venous thrombosis and pulmonary embolism.
She had suffered an episode of septic pulmonary emboli with methicillin-sensitive staphylococcus aureus septicaemia. At the time of this event tomography and a gallium white cell scan revealed tilting of the IVC filter with strut perforation through the IVC and into the third part of the duodenum but no evidence of filter or bypass graft infection.
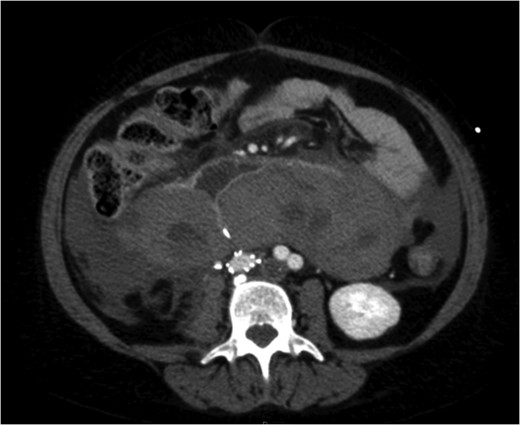
A venous phase abdominal CT demonstrating the end of the IVC filter strut penetrating the wall of the third part of the duodenum.

A coronal section of a venous phase abdominal CT demonstrating the end of the IVC filter strut penetrating the wall of the third part of the duodenum.
The patient's coagulopathy was treated and she underwent a laparotomy and evacuation of a large duodenal haematoma. After division of adhesions, a tense duodenal wall was revealed with splitting of the serosal layer. A large haematoma, of about 500 mls volume, was removed from the subserosal layer without breach of the muscularis. The penetrating strut of the IVC filter was able to be palpated within the duodenal wall but was not on view after haematoma removal. There was considerable inflammation of the retroperitoneum as well as scarring from the previous arterial bypass surgery. There was no contamination of the peritoneum with bowel contents. It was thought preferable to remove the IVC filter via the transvenous route rather than expose the IVC and risk large blood loss and arterial graft contamination in the event of duodenotomy.

Excessive tilting of the IVC filter causes the hook of the filter to appear outside of the lumen of the IVC.
Post operatively the patient's antigoagulation was gradually reintroduced and she made a steady and uncomplicated recovery.
Discussion
Duodenal intramural haematoma can occur secondary to blunt abdominal trauma and this is the most common cause particularly in the paediatric population. Other causes include coagulopathy (inherited and acquired), haematological malignancies, mesenteric venous obstruction, endoscopic procedures, percutaneous drainage procedures, pancreatic pathology, peptic ulcer disease and aortoenteric fistula [1–3]. Bleeding is thought to occur in the submucosal layer [3]. There have been no reports in the literature to our knowledge of IVC filter penetration into the duodenum resulting in a duodenal intramural haematoma. This patient was on warfarin with an INR on presentation of 3.3. This alone may have contributed to her risk of duodenal haematoma.
Duodenal haematoma commonly presents with upper gastrointestinal tract obstruction with abdominal pain and non-bilious vomiting. Other clinical features may include bilious vomiting and obstructive jaundice [3, 4]. The differential diagnosis includes malignancy and there has been one report of a ruptured choledochal cyst being misdiagnosed as a duodenal haematoma [5]. Management is usually non-operative unless there are complicating circumstances [3]. In this case there was free peritoneal blood and a raised white cell count causing concern about duodenal perforation and ongoing bleeding prompting a laparotomy. Conservative therapy with CT or endoscopic guided drainage of the haematoma have also been described [6–8]. In our case, the haematoma consisted of a very firm solid clot under pressure. Non-operative management often requires intravenous nutrition while awaiting clot reabsorption.
Duodenal haematoma has a number of documented causes. We present an unusual case in a complicated patient who required an innovative combination of open surgery and endovascular techniques to achieve a good outcome. Endovascular filter removal can be achieved without bleeding complication even when significant tilting and perforation is present.
Acknowledgements
Nil.
Conflicts of Interest Statement
None declared.
References
- deep vein thrombosis
- pulmonary embolism
- vena cava filters
- intramural hematoma
- computed tomography
- blood coagulation disorders
- aortoenteric fistula
- duodenal obstruction
- epigastric pain
- endoscopy
- hematologic neoplasms
- laparotomy
- peptic ulcer
- shock
- vena cava
- vomiting
- nonpenetrating wounds
- duodenum
- pancreas
- pathology
- duodenal hematoma
- endoscopic surgery
- filters
- emergency evacuation



