-
PDF
- Split View
-
Views
-
Cite
Cite
Carly R.N. Richards, Robert C. McMurray, Erik T. Criman, Margaret E. Clark, Suzanne Gillern, An unusual presentation of a rare disease: posterior reversible encephalopathy syndrome following abdominal sepsis, Journal of Surgical Case Reports, Volume 2016, Issue 11, November 2016, rjw184, https://doi.org/10.1093/jscr/rjw184
Close - Share Icon Share
Abstract
Posterior reversible encephalopathy syndrome (PRES) is an unusual disease of unknown incidence and cause. There are a wide range of associated, predisposing medical causes to include pregnancy, renal failure, immunosuppressive medication administration and hypertension. The diagnosis is made following the radiographic identification of characteristic vasogenic edema in the setting of neurologic impairment. A significant portion of patients will have long-term, if not permanent, sequelae of the disease. We present a patient who developed PRES following a hemicolectomy that was complicated by an anastomotic leak. She went on to a complete recovery following surgical treatment of the leak and supportive care.
INTRODUCTION
Posterior reversible encephalopathy syndrome (PRES) is a rare, poorly understood disease with a number of associated factors but no clearly delineated etiology. Its clinical impact can be devastating and occasionally fatal [1]. Of described cases, it is estimated that greater than one third of patients will never regain baseline neurologic function [2]. Currently there are not any well-established treatment options for PRES [3].
The physiologic causes for PRES are difficult to ascertain in light of the myriad of associated diagnoses and presentations. While PRES is generally associated with hypertension, more recently it has been linked to drug toxicities (e.g. chemotherapy agents, immunosuppressive medications). However, even with these other instigating factors, hypertension likely still plays a significant role. PRES appears to be more common in women though the prevalence data may be skewed by the association of this diagnosis with pregnancy. Presentation is highly variable but generally features a depressed level of consciousness among other sequelae of intracranial hypertension. Other, less common, presentations range from new-onset seizure activity to focal neurologic deficits [4].
The hallmark vasogenic edema on imaging is similar to that found with eclampsia but is unambiguous enough to be diagnostic [5–7]. Significant variation exists, however, such that some authors have observed that this imaging pattern does not necessarily need to be strictly ‘posterior’ and in some cases it is not ‘reversible’ [3, 7, 8]. The differential diagnosis includes stroke, acute demyelinating encephalomyelitis, and cerebral vasculitis.
We present a patient who developed PRES in the immediate post-operative period following complications of a hemicolectomy. Anesthesia and sepsis initially confounded her diagnosis but do not appear to have delayed her treatment and eventual complete neurological recovery.
CASE REPORT
The patient is a 67-year-old woman who presented with a near-obstructing adenocarcinoma of the right colon. She underwent an uneventful laparoscopic-assisted extended right hemicolectomy and was discharged in stable condition on post-operative day 5. She presented to our emergency department (ED) on post-operative day 10 complaining of diffuse abdominal pain, hematemesis and subjective fevers. Computerized tomography (CT) of the abdomen demonstrated a significant amount of free intraperitoneal fluid and associated pneumoperitoneum; she was started on broad spectrum antibiotics and taken to the operating room for an exploratory laparotomy. Upon entry into the abdomen, she was found to have a significant volume of succus and a small anastomotic leak. The anastomosis was resected and an end ileostomy was created. The patient's vital signs were stable and remarkable only for a low grade tachycardia throughout the procedure. She was extubated immediately after the operation. However, due to the patient's persistent obtundation following extubation, she was brought to the intensive care unit (ICU). While her oxygen saturation remained above 95% on supplemental oxygen with both oropharyngeal and nasopharyngeal airways in place, she failed to regain consciousness. When she was noted to be apneic, her respiration was supported with bag valve mask ventilation. The patient was given naloxone, glycopyrrolate and neostigmine to counteract the opioid and paralytic agents received during her procedure without any clinical improvement in her neurologic status. While bedside blood glucose testing was within normal limits, an arterial blood gas demonstrated a profound respiratory acidosis with a pH of 7.03, a PCO2 of 107 and a PaO2 of 375. She was re-intubated for hypercapnic respiratory failure and all sedating medications were held.
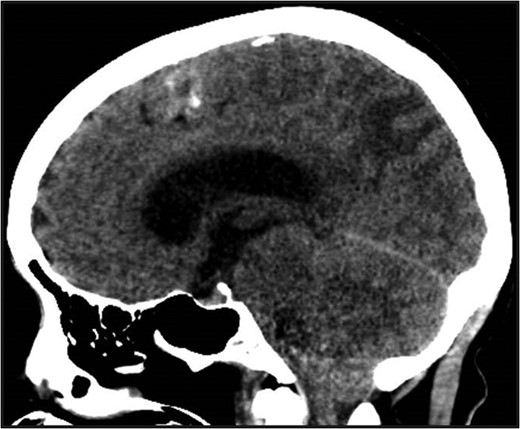
Non-contrast head CT. Non-contrast head CT showing hydrocephalus with tonsillar herniation and vasogenic edema of the parietal and occipital lobes.
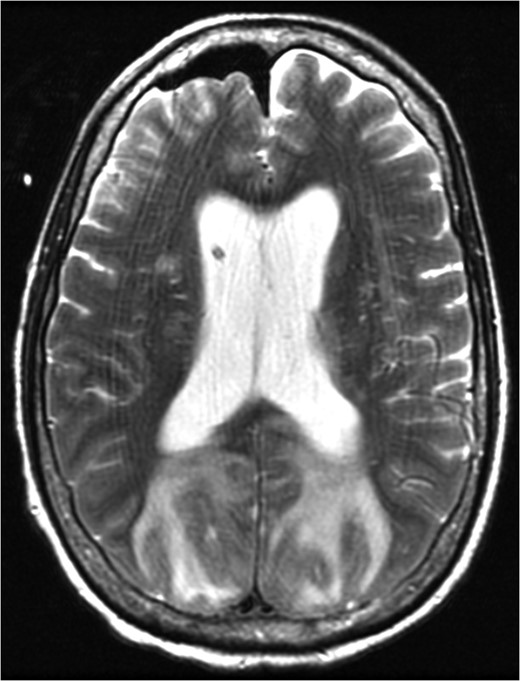
MRI brain at the time of diagnosis, Axial T2 sequence. Vasogenic edema involving the bilateral cerebral hemispheres, with relative sparing of the frontal lobes suggestive of PRES. Pneumocephalus is present secondary to interval placement of an external ventricular drain (seen in the right lateral ventricle).
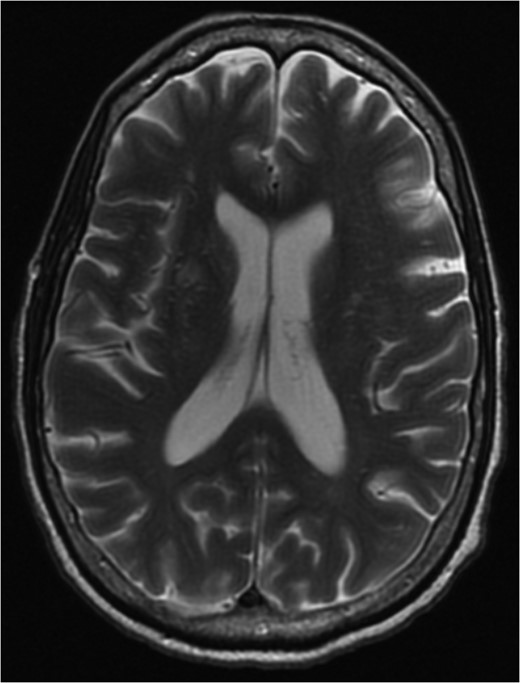
MRI brain 3 months post-diagnosis, Axial T2 sequence. Normalization of imaging with resolution of vasogenic edema and pneumocephalus.
DISCUSSION
PRES was identified as a clinical entity in 1996 by Hinchey et al. In their seminal paper, they described patients with renal insufficiency and hypertension that had extensive bilateral white matter changes within their cerebrum, brainstem, and cerebellum. Of note, seven of the patients they described were on immunosuppressant therapy and were treated in part by decreased or stopped immunosuppression [9]. Prior to Hinchey's formal codification of the diagnosis, this specific set of clinical findings had been attributed to eclampsia given the relative predominance of these findings in pregnant patients with associated hypertension, neurologic sequelae and characteristic vasogenic edema [6]. It is hypothesized that PRES is a direct complication of endothelial injury related to a loss of cerebral autoregulation in the setting of poorly controlled hypertension. Recovery generally occurs within 5–6 days with supportive care including maintenance of normotension, treatment of sepsis and the cessation of any offending medications [1].
While PRES has been associated with sepsis, colorectal cancer and a history of chemotherapy administration; fulminant presentation in the immediate post-operative period in the setting of normotension has not been described. While subtle manifestations were seen in two of the four total perioperative cases identified, these patients exhibited mild to moderate new onset hypertension in the immediate post-operative period [10]. In the case we describe, the patient was obtunded from the immediate postoperative period until diagnosis and subsequent management aimed at reducing intracranial hypertension. We theorize that the systemic vasodilation and capillary leak associated with this patient's abdominal sepsis was exacerbated by the induction of anesthesia and precipitated PRES. Despite her resultant vasogenic edema and intracranial hypertension progressing to tonsillar herniation, timely surgical intervention and optimal medical management facilitated a complete neurologic recovery.
DISCLOSURE STATEMENT
The views expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Department of the Army, Department of Defense, or the US Government.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES
- pregnancy
- hypertension
- diagnostic radiologic examination
- immunosuppressive agents
- kidney failure
- surgical procedures, operative
- diagnosis
- vasogenic brain edema
- abdominal sepsis
- anastomotic leak
- medication management
- reversible posterior leukoencephalopathy syndrome
- neurologic deficits
- supportive care
- rare diseases



