-
PDF
- Split View
-
Views
-
Cite
Cite
Sonwabile Gonya, Andile Mbatha, Nondabula Moyeni, Basil Enicker, Retained garden fork following cranial stab injury, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv175, https://doi.org/10.1093/jscr/rjv175
Close - Share Icon Share
Abstract
Retained garden fork is a rare complication of penetrating cranial trauma. Retained knife blade is the most commonly reported presentation. We report an unusual case of a 30-year-old male patient treated at our institution, who presented with a retained garden fork following a stab to the head, with no associated neurological deficits. Computerized tomographic scan of the brain was performed preoperatively to assess the trajectory of the weapon and parenchymal injury. A craniectomy was performed to facilitate removal of the weapon in the operating theatre under general anaesthesia. Intravenous prophylactic antibiotics were administered pre- and postoperatively to prevent septic complications. The patient recovered well and was discharged home.
INTRODUCTION
Penetrating cranial injuries are common in South Africa (SA) [1]. Transcranial retained foreign bodies are often a sequela of these assaults. Previous reports emanating from SA have reported on retained cranial knife blades and these injuries can be associated with significant morbidity and mortality [2]. We report an unusual case of a patient who presented with a retained garden fork following a stab to the head.
CASE REPORT
A 30-year–old male patient was stabbed in the head with a garden fork following a dispute with a neighbour. He was initially assessed at his local hospital, which referred him to our neurosurgery unit for further management. On arrival, he was haemodynamically stable and was noted to have a retained garden fork in the left frontal area. His Glasgow Coma Scale (GCS) was 14/15, with no associated neurological deficits. He was noted to have left peri-orbital swelling, but vision was intact. There was no active bleeding from the wound and no other associated injuries. He was intoxicated at the time of examination and had a generalized tonic–clonic seizure in the emergency department, which was aborted. He was loaded with phenytoin and put on maintenance therapy. A computerized tomographic (CT) scan of the brain showed a retained garden fork in the frontal area (Fig. 1). The garden fork prong had penetrated the left frontal cortex; however, it caused a lot of artefact making visualization of parenchymal tissue damage difficult to appreciate (Fig. 2). Tetanus toxoid was administered and he was taken to the operating theatre for removal of the garden fork under general anaesthesia. At induction, intravenous first-generation cephalosporin and metronidazole were administered for prophylaxis.
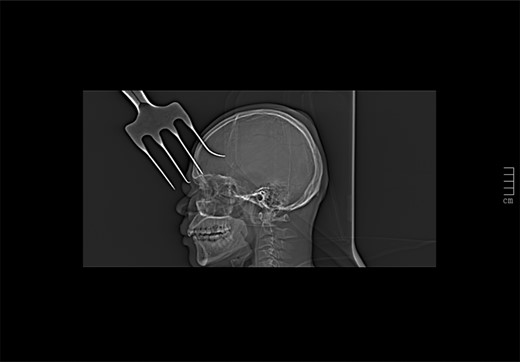
CT scout view showing a retained garden fork in the frontal area.
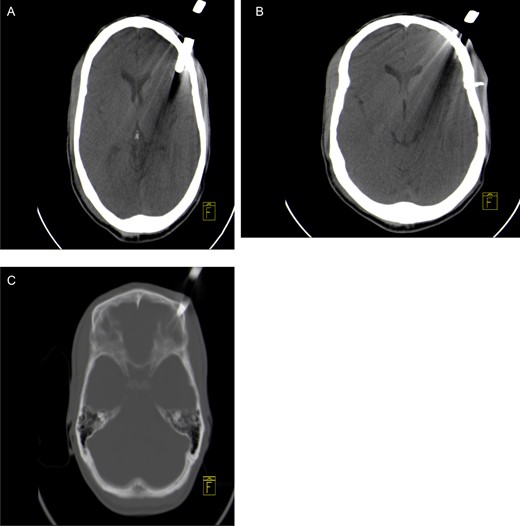
Axial non-contrast CT brain scan showing a garden fork prong in the left frontal parenchyma with associated artefact (A) and loose bone fragment in left frontal soft tissue (B). Axial CT bone window showing left frontal bone fracture caused by the fork (C).
The left frontal wound was extended and a craniectomy was performed around the embedded fork prong. The fork was removed in-line with its trajectory. Intraoperatively, a left frontal fracture with associated dural defect and contused brain were noted. The wound and injured brain tissue were irrigated thoroughly, ensuring removal all debris. A pericranium graft was used to close the dural defect and the wound was closed in layers. Postoperatively intravenous antibiotics were continued for 5 days. There were no signs of intracranial infection postoperatively and no further seizures were reported during the admission period. The GCS improved to 15/15 and he was discharged home on Day 6.
DISCUSSION
Retained garden fork is an extremely rare complication of penetrating cranial trauma. In addition to injury to the underlying brain tissue and vasculature, it can result in gross contamination of the wound tract with soil, small stones and grass, as this is an outdoor instrument.
A CT brain scan is the investigation of choice before embarking on surgical removal to assess damage to underlying parenchyma and trajectory of the weapon. An angiogram is indicated if the weapon traverses an area of major vasculature, which was not the case in our patient. The goals of treatment are 2-fold, i.e. first to prevent further brain and soft tissue injury, and secondly, to prevent secondary infections such as meningitis, empyema and cerebral abscess which can occur when the dura mater is breached and are associated with morbidity and mortality [3].
To achieve these goals, it is imperative that a tetanus toxoid and prophylactic intravenous antibiotics are administered preoperatively to counter the effects of Clostridium species, among the many organisms that are commonly found in the soil and can cause tetanus and intracranial sepsis.
The garden fork should be removed in the operating theatre under general anaesthesia where the wound is thoroughly debrided taking care to remove all the debris that are deposited into the wound during the assault, as well as loose bone fragments and devitalized tissue. In our unit, we subscribe to a 5-day course of postoperative prophylactic intravenous antibiotics in patients with wounds contaminated by soil to prevent intracranial sepsis, which did not manifest in our patient.
Retained garden fork injury is rare, but requires emergent attention to limit further tissue damage and associated septic complications. It is imperative for neurosurgeons based in referral trauma centres to be aware of different patterns of penetrating cranial injuries and to formulate guidelines that manage these injuries in an effective manner to ensure a good outcome [4].
CONFLICT OF INTEREST STATEMENT
None declared.



