-
PDF
- Split View
-
Views
-
Cite
Cite
Elroy P. Weledji, M. Ngowe Ngowe, Divine M. Mokake, Vincent Verla, Post-traumatic pancreatic pseudocyst managed by Roux-en-Y drainage, Journal of Surgical Case Reports, Volume 2015, Issue 8, August 2015, rjv094, https://doi.org/10.1093/jscr/rjv094
Close - Share Icon Share
Abstract
A pancreatic pseudocyst is a collection of serous fluid in relation to the pancreas following acute pancreatitis. If pancreatography is performed, most pseudocysts will be found to have a connection with the pancreatic ductal system. Most will resolve spontaneously but clinically significant pseudocysts (∼5%) may require surgical intervention. Surgical (laparoscopic or open) direct drainage of pancreatic pseudocysts into the upper gastrointestinal tract is the mainstay of treatment with the possibility of pancreatic resection if malignancy is suspected. We report a persistent post-traumatic pancreatic pseudocyst of 8-year duration, despite recurrent percutaneous aspiration that was finally managed by a Roux-en-Y drainage.
INTRODUCTION
Pancreatic pseudocysts developed in 23% of patients following pancreatic trauma and endoscopic retrograde pancreatography demonstrated duct injury in half of these (grade III pancreatic injury) (Table 1) [1–3]. Percutaneous radiologically guided drainage is an alternative but has a failure rate of 55%, and it is not suitable for the communicating mature pseudocyst [4]. External drainage has the disadvantage that it may introduce infection and leave the patient with an external fistula [1, 4, 5]. Endoscopic or endoscopic ultrasound (EUS)-guided drainage of pancreatic pseudocyst that bulges into the gut lumen via a cystgastrostomy, cystduodenostomy or transpapillary method is another alternative, but requires careful patient selection and skill [6]. These methods are gaining popularity, but no randomized trials have been done to compare them with traditional methods [1, 5–7].
| Gradea . | Type of injury . | Description of injury . |
|---|---|---|
| I | Haematoma | Minor contusion without duct injury |
| Laceration | Superficial laceration without duct injury | |
| II | Haematoma | Major contusion without duct injury or tissue loss |
| Laceration | Major contusion without duct injury or tissue loss | |
| III | Laceration | Distal transection or parenchymal injury with duct injury |
| IV | Laceration | Proximal transection or parenchymal injury involving ampulla |
| V | Laceration | Massive disruption of pancreatic head |
| Gradea . | Type of injury . | Description of injury . |
|---|---|---|
| I | Haematoma | Minor contusion without duct injury |
| Laceration | Superficial laceration without duct injury | |
| II | Haematoma | Major contusion without duct injury or tissue loss |
| Laceration | Major contusion without duct injury or tissue loss | |
| III | Laceration | Distal transection or parenchymal injury with duct injury |
| IV | Laceration | Proximal transection or parenchymal injury involving ampulla |
| V | Laceration | Massive disruption of pancreatic head |
Proximal pancreas is to the patient's right of the superior mesenteric vein.
aAdvance one grade for multiple injuries up to grade III.
| Gradea . | Type of injury . | Description of injury . |
|---|---|---|
| I | Haematoma | Minor contusion without duct injury |
| Laceration | Superficial laceration without duct injury | |
| II | Haematoma | Major contusion without duct injury or tissue loss |
| Laceration | Major contusion without duct injury or tissue loss | |
| III | Laceration | Distal transection or parenchymal injury with duct injury |
| IV | Laceration | Proximal transection or parenchymal injury involving ampulla |
| V | Laceration | Massive disruption of pancreatic head |
| Gradea . | Type of injury . | Description of injury . |
|---|---|---|
| I | Haematoma | Minor contusion without duct injury |
| Laceration | Superficial laceration without duct injury | |
| II | Haematoma | Major contusion without duct injury or tissue loss |
| Laceration | Major contusion without duct injury or tissue loss | |
| III | Laceration | Distal transection or parenchymal injury with duct injury |
| IV | Laceration | Proximal transection or parenchymal injury involving ampulla |
| V | Laceration | Massive disruption of pancreatic head |
Proximal pancreas is to the patient's right of the superior mesenteric vein.
aAdvance one grade for multiple injuries up to grade III.
CASE REPORT
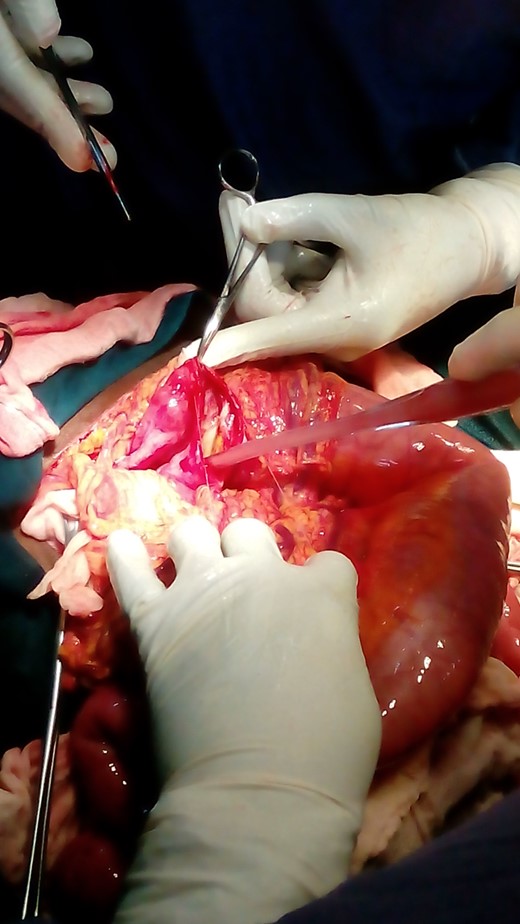
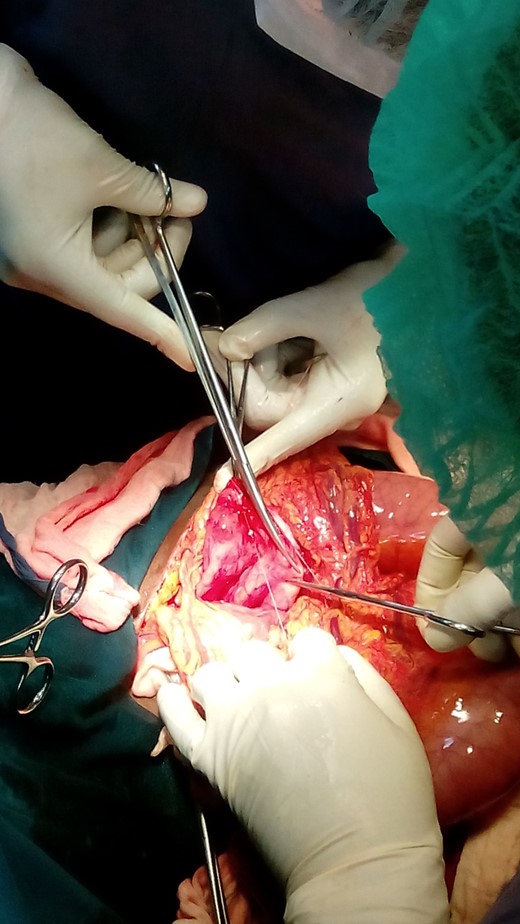
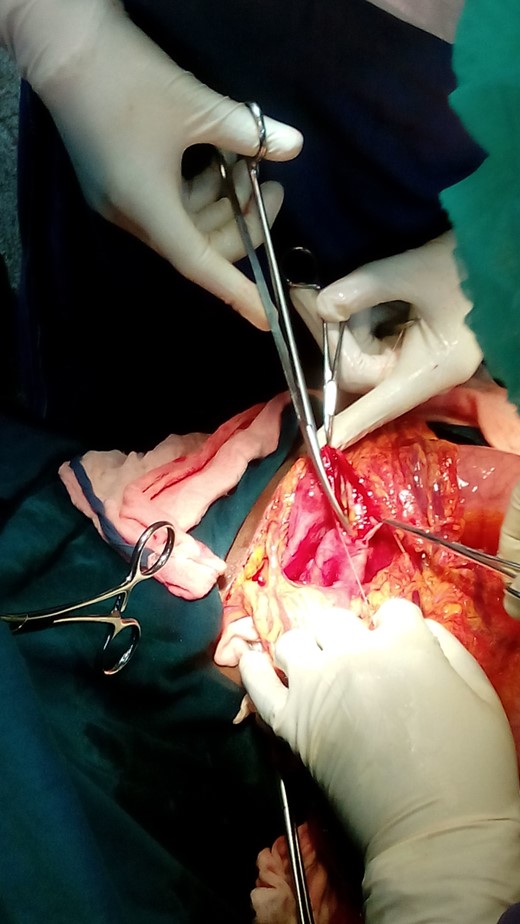
A 27-year-old African woman who is non-alcoholic presented with an enlarging epigastric mass of 8-year duration following blunt abdominal trauma from a fall off a motorbike. This mass persisted despite percutaneous aspiration. Apart from post-prandial bloating, early satiety and difficulty while lying supine, she was clinically well. Physical examination revealed a tense, forward bulging, epigastric mass of ∼20 cm diameter with a palpable smooth upper border but impalpable lower border. The mass did not move with respiration as it appeared fixed to the retroperitoneum. There was no organomegaly nor palpable lymphadenopathy. Blood tests revealed a raised serum amylase of 151 U/L (normal 70–300 U/L) and a haemoglobin level of 11 g/dl (normal 12–15). A computed tomography (CT) scan confirmed a retroperitoneal cystic mass within the body and tail of pancreas with the main differential diagnosis of a pancreatic pseudocyst (Fig. 1). The patient consented for an internal drainage of the pseudocyst. Under general anaesthesia, a nasogastric tube was passed because gastric emptying is often impaired. Following an upper midline incision, the lesser sac was entered through the gastrocolic omentum and the large, tense, smooth thick-walled mature cyst of ∼25 cm in diameter was found attached to the body and tail of the pancreas. It bulged inferiorly into the transverse mesocolon causing a localized dilatation (Fig. 2). A laparotomy revealed a normal gall bladder and excluded gallstones as a possible cause of the pancreatitis. Taking care to avoid vessels densely adherent to the pseudocyst, a 5-cm incision of the anterior wall of the cyst with cutting diathermy drained ∼2.8 l of thick creamy fluid consistent with pancreatic juice. Loculi within the cyst were broken down with the suction catheter (Fig. 3). As malignancy was not suspected, a sample was not analysed. The upper end of a retrocolic Roux loop of jejunum with its closed end was approximated to the front of the cyst without tension (Fig. 4). A generous side-to side two - layer anastomosis between the opening into the cyst and a longitudinal jejunostomy was fashioned. This entailed an inner ‘all coats’ continuous suture of non-absorbable material (nylon) and an outer layer of interrupted absorbable (vicryl) to ensure serosal apposition (Fig. 5). Intestinal continuity was restored by jejunojejunostomy at the base of the Roux loop. The mesocolic and jejunojejunal defects were closed to avoid internal hernias. The distended transverse colon was decompressed by suction aspiration of colonic gas using a 22-g i.v. cannula through the taenia so as to allow a safe abdominal closure. The patient lost ∼200 ml of blood and received a unit of whole blood intraoperatively. Following abdominal lavage, a corrugated (R) paracolic drain was inserted and the midline wound closed by a mass closure technique with a monofilament non-absorbable 1.0 nylon, and interrupted nylon sutures for the skin. A dry dressing was applied. Postoperative recovery was uneventful. The nasogastric tube was removed on the second day as her serum amylase was within the normal range. Her bowels moved on the second day and the drain removed on the fifth postoperative day. The patient was discharged on the 10th postoperative day and long-term follow-up planned.
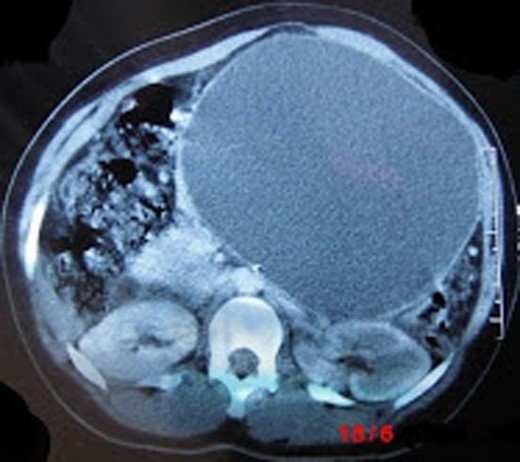
CT showing a large pancreatic pseudocyst in the body and tail of pancreas bulging into the anterior abdominal wall and displacing loops of the small bowel.

Mobilized bulging pancreatic pseudocyst with distended transverse colon inferiorly.
Approximation of long limb of Roux to the pseudocyst without tension.
DISCUSSION
Traumatic pancreatic pseudocysts associated with peripheral ductal injury may resolve spontaneously or be treated successfully by percutaneous aspiration, whereas those associated with injuries to the proximal duct (head of pancreas) require internal drainage by Roux-en-Y cystjejunostomy [3]. The optimal point of drainage can be inferred from the CT scan, where the cyst wall is thin and extrapancreatic but careful intraoperative assessment for dependent drainage is desirable [1, 5, 8, 9]. A common misdiagnosis for pseudocysts are mucinous cystic tumours, which make 40–50% of pancreatic cysts and are radiologically similar to pseudocysts [10]. A sample of the pseudocyst wall is sent routinely for histological examination to exclude the presence of an epithelial lining and confirm that the collection was inflammatory rather than neoplastic [1, 5]. A cystgastrostomy would effectively drain a retrogastric pseudocyst and prevent reaccumulation of fluid [1]. An inferior pseudocyst that bulges through the transverse mesocolon as in this case is preferentially drained into a Roux loop of jejunum. This obtains dependent drainage and excludes the cyst contents from food and bile, and should prevent activation of the pancreatic secretions until they are within the jejunum [5]. More rarely, those at the head of the pancreas may be drained into the duodenum by a cystoduodenostomy, and those related to the tail of the pancreas are best managed by distal pancreatectomy with a splenectomy [2, 3, 5]. If possible, surgical intervention should be avoided until the pseudocyst is at least 6 weeks old, by which time the wall will usually be fibrotic enough to hold sutures [1, 5]. Cutting out of sutures in the pseudocyst wall increases the risk of pancreatic ascites. If this occurs the anastomosis should be abandoned, and external drainage carried out [5]. Continuous sutures are mostly used for cystgastrostomy so as to control haemorrhage from the pseudocyst wall or inflamed wall of the stomach [1, 5]. Postoperative complications may include a flare up of acute pancreatitis, haemorrhage from the suture lines or from the vessels of the wall of the pseudocyst as it collapses, pancreatic ascites, external pancreatic fistulae and recurrent pseudocyst formation [1, 3, 5]. The reported pseudocyst recurrence rate of 10–20% following internal drainage is due either to inadequate stoma size, failure to break down loculi within the pseudocyst or to a persistent communication to the pancreatic duct [5, 8]. The latter is characteristic of the post-traumatic pancreatic pseudocyst due to associated duct injury [3]. After excluding a mucinous cystic tumour via an EUS-guided fine needle aspiration of cyst fluid for analysis, a pancreatic sphincterotomy with or without stenting of the main pancreatic duct disruption would manage a persistent communicating pancreatic pseudocyst [1, 3, 5, 6, 9].
Written informed consent was obtained from the patient for publication of the case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal.
AUTHORS' CONTRIBUTION
E.P.W. was the main author and part of the surgical team, M.N.N. was the Chief surgeon, D.M.M. was part of the surgical team and V.V. was the anaesthetist.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENT
We thank the medical students who provide the images and the theatre and surgical nursing staff of the Regional Hospital Buea for the perioperative care of the patient.



