-
PDF
- Split View
-
Views
-
Cite
Cite
John R. Gusz, Lauren M. Wright, Intestinal obstruction secondary to left paraduodenal hernia, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv090, https://doi.org/10.1093/jscr/rjv090
Close - Share Icon Share
Abstract
An internal hernia—congenital or acquired—is a protrusion of bowel through an opening in the peritoneum or mesentery. Internal hernias are the etiology of <2% of intestinal obstructions, with paraduodenal hernias being the most common type of congenital internal hernia. We report a case of a left paraduodenal hernia (LPDH) combined with partial small bowel obstruction in a 69-year-old male with recurrent abdominal pain of 2 years duration and no previous abdominal surgeries. An abdominal computed tomography scan showed an agglomeration of small bowel loops in the left upper quadrant but failed to yield a clear diagnosis. Surgical intervention provided definitive diagnosis and treatment of the LPDH. We additionally review the literature regarding anatomy, pathogenesis, diagnosis and treatment of this uncommon hernia. Intestinal obstruction secondary to an internal hernia is a rare entity; however, delayed diagnosis and surgical intervention may result in significant morbidity and mortality.
INTRODUCTION
An internal hernia—congenital or acquired—is a protrusion of viscera through an opening in the peritoneum or mesentery [1]. Internal hernias are the etiology of <2% of intestinal obstructions, with paraduodenal hernias being the most common type of congenital internal hernia [2]. Paraduodenal hernias result from the failure of mesenteric fusion with parietal peritoneum and malrotation of midgut and subsequent development of potential space in the left paraduodenal fossa [3]. Symptoms associated with paraduodenal hernias are generally nonspecific; therefore, diagnosis is most commonly due to incidental findings on imaging or at laparotomy/laparoscopy [4]. Due to the fact that paraduodenal hernias can lead to bowel obstruction, ischemia and perforation with a high mortality, an elevated index of suspicion paired with diagnostic imaging/procedure is essential to making a timely and correct diagnosis [5, 6]. In this review, we discuss the clinical presentation and management of small bowel obstruction secondary to a left paraduodenal hernia (LPDH).
CASE REPORT
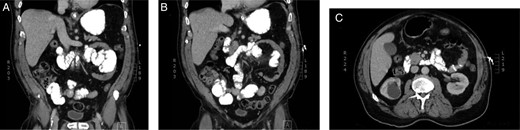
A 69-year-old Caucasian male was admitted to the hospital due to abdominal pain of ∼20 h duration. He described the abdominal pain as ‘achy’, constant, diffuse and with no radiation. Associated nausea and similar episodes of pain over the past 2 years were noted. Patient denied vomiting, fever, weight loss or change in bowel habits or urination. Only significant past medical and surgical history being prostate cancer treated with radiation. On examination, the patient appeared in mild distress and vital signs within normal limits. Physical exam revealed a moderately distended abdomen with an initially incarcerated umbilical hernia. The hernia was able to be manually reduced, which resulted in slight decrease of pain. Hematological and biochemical studies were within normal limits, and a computed tomography (CT) scan demonstrated borderline dilated loops of proximal small bowel; however, no transition point was identified. After discussion with a radiologist, a partial small bowel obstruction secondary to possible LPDH was confirmed (Fig. 1).
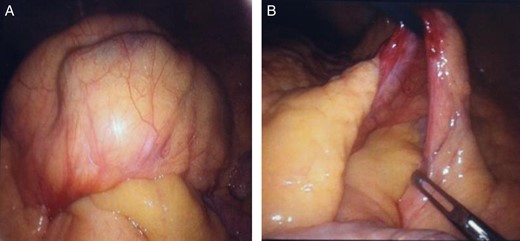
The patient was taken to the operating room within 12 h of hospital admission where a diagnostic laparoscopy was performed. While running the bowel, a hernia sac was discovered arising from a defect to the left of the fourth part of the duodenum, consistent with a LPDH (Fig. 2). An aggregation of intestinal loops was herniated through the defect into the fossa of Landzert. The bowel was then easily reduced using bowel graspers, and a scar was noted to be tacking the orifice to the mesentery, trapping the first part of the jejunum. The bowel was intermittently dilated and compressed. Due to a section of reduced bowel remaining visibly dusky, a small midline laparotomy was performed to allow tactile examination of the bowel. After the mild ischemia was observed to have reverted and no further obstruction was ensured, the bowel was returned to the abdominal cavity and the LPDH orifice was closed primarily by fixing the root of the mesentery to the posterior parietal peritoneum.
The postoperative course was uneventful with complete resolution of abdominal pain. The patient was discharged on the seventh postoperative day, with instructions for resumption of normal daily activities. Follow-up at 1 month revealed no recurrence of clinical symptoms.
DISCUSSION
Internal hernias are a rare pathology of intestinal obstruction, accounting for <2% [2, 4]. Paraduodenal hernias, being the most common type of congenital internal hernias, are responsible for ∼1% of small bowel obstructions [4]. LPDHs have been referred to by various terms: Treitz retroperitoneal hernia, hernia of the fossa of Landzert, mesentericoparietal hernia of Logace and hernia into the descending mesocolon of Callader [6]. Overall, a LPDH is three times more common than a right paraduodenal hernia (Waldayer's hernia) [2, 5, 7]. LPDH occurs when small bowel, usually jejunum, prolapses posteroinferiorly into the defect of the left paraduodenal fossa. Landmarks of the fossa of Landzert being left of the fourth part of the duodenum, anterior to the posterior peritoneum and posterior to the inferior mesenteric vein and left branches of the middle colic artery [3, 8, 9].
In congruency with presented case, median age range at diagnosis is fourth and sixth decades, and the male to female ratio is 3:1 [2]. In this review, patients typically presented with signs and symptoms compatible with bowel obstruction secondary to incarceration, strangulation or necrosis [5]. Abdominal pain and associated symptoms being generally nonspecific, with 50% recounting recurring abdominal pain and occasionally a palpable mass [2, 5]. Most effective diagnostic tool for LPDHs is a CT scan, with typical appearance being an encapsulated sac containing dilated small bowl loops at the duodenojejunal junction with mass effect compression of the posterior stomach and distal duodenum. Additionally, engorgement and distention of the mesenteric vessels will commonly shift the mesenteric trunk to the right and displace the transverse colon downward [1, 4].
Patients with a LPDH have a 50% lifetime risk of hernia incarceration with 20–50% mortality for acute presentations; therefore, after the diagnosis of a LPDH, operative management is recommended regardless of symptoms [4]. In this review, laparoscopic and laparotomy repair is documented to be appropriate, using basic principles of hernia repair—reduction of contents, restoration of anatomy and repair of the defect primarily or with mesh [5]. Alternative techniques of widening the hernia orifice and division of the inferior mesenteric vessels at the orifice can be implemented in cases where defect prevents repair using sutures or if reduction of contents from the fossa is a challenge [2, 3, 5, 6].
Intestinal obstruction secondary to an internal hernia is a rare entity; however, delayed diagnosis and surgical intervention may result in significant morbidity and mortality [2, 4, 6]. Therefore, in accordance with the above-noted literature and the surgical and clinical success of this case, it is important to include a paraduodenal hernia in the differential diagnosis of a patient presenting with small bowel obstruction and no history of abdominal surgery [10].
CONFLICT OF INTEREST STATEMENT
None declared.



