-
PDF
- Split View
-
Views
-
Cite
Cite
Adnan A. Sheikh, Olorundi Rotimi, Deepa Jacob, Racheal Hyland, Peter M. Sagar, Transitional cell carcinoma arising in a tailgut cyst, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv085, https://doi.org/10.1093/jscr/rjv085
Close - Share Icon Share
Abstract
Malignant transformation in tailgut cysts (TGCs) is extremely rare, with no reports of transitional cell carcinoma arising in them in the UK literature. Here, we discuss a case of a patient with a malignant TGC encapsulating the rectum. This case report highlights the pathological and diagnostic considerations and discusses its management.
INTRODUCTION
Tailgut cysts (TGCs) in the presacral region are extremely rare entities [1, 2]. These retrorectal tumours arise in most cases from tissue remnants of embryological origin [3, 4]. They are primarily derived from cells of dermoid and enterogenous linage and histologically contain mucous-secreting epithelium, which demonstrate an inflammatory and/or infective tissue response owing to microtrauma [3].
Clinical presentation of TGCs is varied, with a preponderance to females, and these tumours often present as perianal fistula or abscesses in either the perianal or pilonidal area [5]. Symptoms vary, ranging from specific symptoms such as constipation, incontinence and sexual dysfunction to vague symptoms of non-specific pelvic and back pain [4]. Malignant transformation of TGCs is extremely rare, with 23 reported cases in the literature, the greater proportion being adenocarcinoma [1, 6].
We present a case of a 35-year-old female with a transitional cell carcinoma arising in a TGC encasing the rectum.
CASE REPORT
A 35-year-old woman attended as an emergency admission with lower abdominal pain. Her clinical and haemodynamic parameters were in keeping with acute appendicitis, and a diagnostic laparoscopy was undertaken that identified an adenexal mass. A subsequent computed tomography (CT) and magnetic resonance imaging (MRI) of her abdomen and pelvis demonstrated a mass arising in the right retrorectal space comprising of complex papillary nodules, breaching the capsule in which it was contained. The lesion filled the entire mesorectal envelope and was in contact with the vagina and left levator plate (Fig. 1A and B). Both MR and CT appearances were in keeping with malignant change in a retrorectal duplication cyst (TGC) with extra-capsular spread.
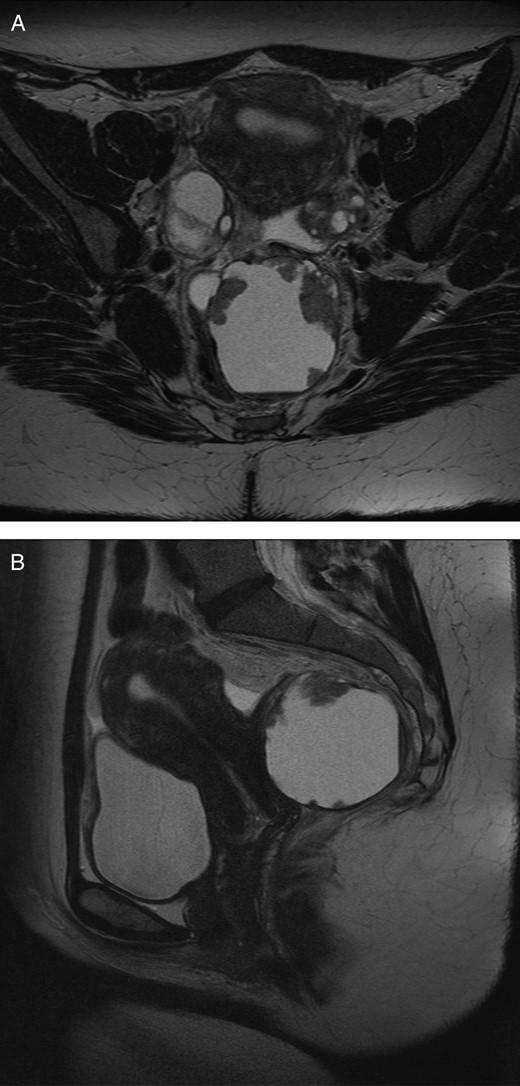
(A) Axial MRI image of pelvis demonstrating retrorectal cyst. (B) Sagittal MRI image of pelvis demonstrating retrorectal cyst.
Owing to invasion of the mesorectal envelope and encasement of the rectum, this patient underwent a laparoscopic low anterior resection with a defunctioning ileostomy. The cyst was taken enbloc with the rectum and lateral pelvic side wall. Postoperatively the patient made a good recovery and was discharged home subsequently in 5 days. Histology of the specimen demonstrated a transitional cell carcinoma arising in a TGC encasing the rectum with good clearance of the resection margins (Fig. 2A–C).
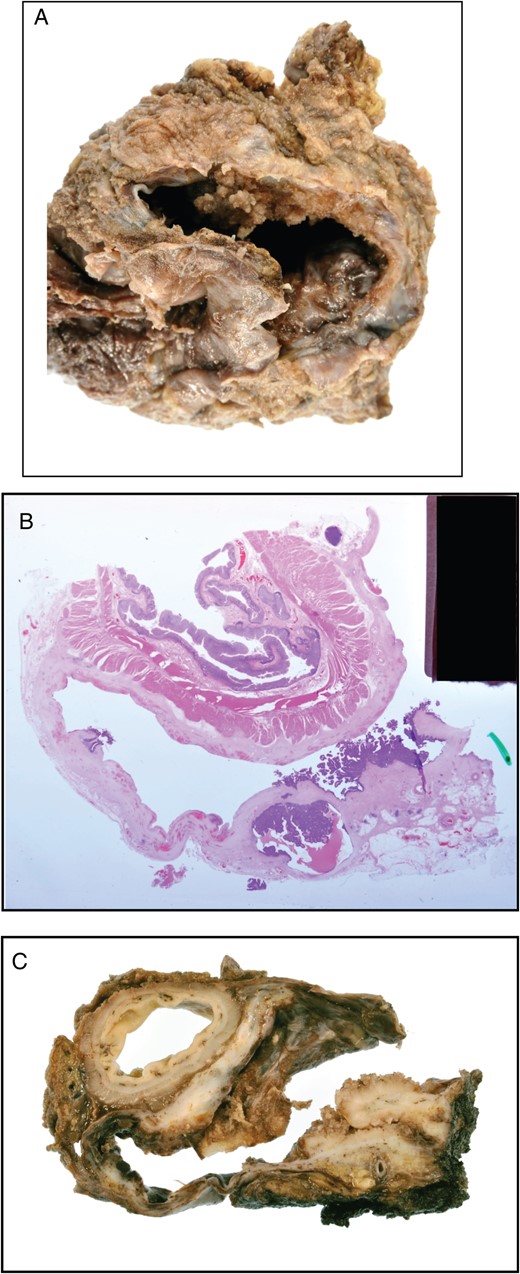
(A) Pathological specimen demonstrating the cyst with transitional cell epithelium. (B) Pathological specimen demonstrating the cyst and rectum. (C) Histology demonstrating the cyst invading the rectum.
DISCUSSION
TGCs are congenital retrorectal tumours, present in the presacral space arising from primitive tail gut cyst remnants. Management is challenging owing to their location in the presacral space, which is bounded anteriorly by the rectum, posteriorly by the peritoneal reflection and sacral plexus, inferiorly by the levator ani and coccygeal muscle and laterally by the pelvic side wall comprising of the internal iliac vasculature [5].
Retrorectal tumours represent a diverse mix, ranging from chordomas to schwannomas to TGCs. A majority of these are well defined, with a benign appearance on histology and imaging. Malignant transformation in TGCs is extremely rare, with only a handful of reported cases in the literature, the majority being squamous cell carcinoma, adenocarcinoma and carcinoid in nature [1, 3, 4, 7].
Diagnosis is challenging, requiring a multidisciplinary team approach with cross-sectional imaging in the way of CT and MRI being of paramount importance in delineating these lesions. Sensitivity of T2-weighted MRI is high, particularly in experienced hands where differentiation between malignant and benign lesions can be done [7, 8]. This precludes the need for preoperative histological diagnosis, which remains an area of debate amongst experts. The authors do not advocate core biopsy owing to the risk of seedling in the case of malignant transformation and of recurrence in the case of cell spillage into the pelvic cavity. Moreover, yield of biopsy tissue diagnosis is often poor resulting in false-negative results. In the authors’ experience, excision of the TGC in its entirety is the best way to confirm tissue diagnosis [2, 6, 8].
Retrorectal tumours can be removed both through an open and laparoscopic approach, with the authors having undertaken over 76 primary procedures with a further series of 15 recurrent retrorectal tumour excisions [8]. Type of surgical approach depends on the level of the lesion, with low tumours below S3 level being approached from the perineum. Lesions above S3 benefit from an abdominal approach or at times a combined approach [2, 5, 8]. A robust imagining and MDT service is key to the management of these lesions as invasion of adjacent structures, i.e. rectum and lateral pelvic side wall will dictate whether or not resection of the rectum or pelvic vasculature is needed.
Histologically, TGCs comprise of a wide range of epithelia containing both endodermal and mesenchymal tissues [1]. Squamous and columnar epithelia are common with no reported cases of transitional cell carcinoma arsing in the retrorectal space in the UK literature [4]. In our particular case, the cancer arising in the cyst was invasive encapsulating the rectum with direct invasion into the mesorectum. The operative findings were in keeping with the patients' symptoms of difficulty in defecation and tenusmus. The presence of transitional cell carcinoma in the retrorectal space could be mistaken for a cancer arising in the ureters at the trigone of the bladder, which in this particular case were normal bilaterally. Malignant transformation in transitional cells in a duplication cyst can theoretically develop owing to lack of exposure to urine, as described by Moloney et al. in a defunctionalized bladder; this, however, is only theoretical with no direct evidence of occurrence in our case [9].
Review of this case in both the urological and colorectal oncology multidisciplinary team meetings concluded an expectant management protocol with annual imaging for the first 3 years postoperatively, followed by a CT scan at 5 years prior to discharge from clinical follow-up.
TGCs are rare and in a majority of cases are benign cystic lesions. They can be removed either through a perineal or abdominal approach with surgical management being challenging owing to their location. A multidisciplinary team approach is therefore essential to achieve good outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



