-
PDF
- Split View
-
Views
-
Cite
Cite
Tobias Huber, Markus Paschold, Alexander J. Eckardt, Hauke Lang, Werner Kneist, Surgical therapy of primary intestinal lymphangiectasia in adults, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv081, https://doi.org/10.1093/jscr/rjv081
Close - Share Icon Share
Abstract
Primary intestinal lymphangiectasia (PIL) is a rare disorder, especially in adults. It causes a local disruption of chylus transport and is part of the exudative gastroenteropathies. Conservative therapy includes dietary measures or somatostatin medication. Taking the differential diagnosis of PIL into consideration is a major challenge, since patients suffering from PIL may present with diarrhoea and lymphedema or chylous ascites. This can be explained by the chronic lymphedema of the bowel leading to dilation of the vessels (intraluminal loss) and sometimes even to a rupture (peritoneal loss). Push–pull enteroscopy and capsule endoscopy are the proper interventional diagnostic tools to discover PIL. Exploratory laparoscopy may be useful in unclear cases. Surgical resection of the altered intestine has been described with positive results. Exploratory laparoscopy may even be a diagnostic tool in unclear cases. Resection of the altered intestine is a treatment option in symptomatic and treatment-refractory cases.
INTRODUCTION
Primary intestinal lymphangiectasia (PIL) is a rare disorder of the intestine that is part of exudative gastroenteropathies and has primarily been described in children by Waldmann et al. Overall, <200 cases of PIL have been described. Reports in adulthood are even more rare [1–3].
Diagnosis of PIL is quite difficult for gastroenterologists because the symptoms vary from shortness of breath, chronic lymphedema or diarrhoea to immunodeficiency with opportunistic infections or osteomalacia. Some patients may even present with pleural effusion, chylous ascites, jejunal ileus or acute abdomen [2, 4]. Thus, taking the possible differential diagnosis of PIL into consideration is a major challenge.
Push–pull enteroscopy and capsule endoscopy of the small intestine are described as the method of choice when a reasonable suspicion for PIL is given [5]. Magnetic resonance imaging (MRI) can be a helpful tool in the process of diagnosis [6]. Primary treatment of PIL in adults is usually conservative with a low-fat diet, a substitution of medium-chain triglycerides as well as treatment with somatostatin to reduce the intestinal lymph flow [7]. However, surgical resection of an affected intestinal segment has also been described with positive results [2, 8, 9].
CASE REPORT
A 51-year-old male patient had been suffering from a massive lymphedema of the lower extremities also including the scrotum for almost 20 years. Despite consequent lymph drainage up to four times per week, the patient showed progressive symptoms with suddenly occurring diarrhoea, a massive impairment of physical capabilities and a severe reduction in the quality of life. The patient's weight was consistent with 110 kg at a height of 184 cm [body mass index (BMI): 32.5 kg/m²]. Pulmonary, cardiac and hepatological diagnostics showed no underlying disease. Gastroscopy and colonoscopy gave no pathological findings. The only exceptional result was a protein deficiency with a chronic lowered total serum protein (47 g/l; normal range 64–84 g/l). Gel serum electrophoresis showed a general protein deficiency.
Since conservative treatment with lymph drainage showed no improvement of the patient's symptoms, further diagnostic steps including a push–pull enteroscopy revealed the PIL of the jejunum to an extent of about 50 cm (Supplementary Video 1). Subsequent capsule endoscopy confirmed the limited involvement of the proximal to mid jejunum.
Due to the extensive impairment of the patient and the therapy-refractory course, the indication to exploratory laparoscopy with segmental intestinal resection was given.
During the laparoscopic operation, an extensive part of the small intestine appeared macroscopically clearly altered (Supplementary Video 2). Thus, the laparoscopic-assisted resection of the conspicuous intestine (95 cm) with end-to-side anastomosis was performed.
Histopathological analysis confirmed the PIL with dilated submucosal and subserosal lymphatic vessels (Fig. 1a and b).
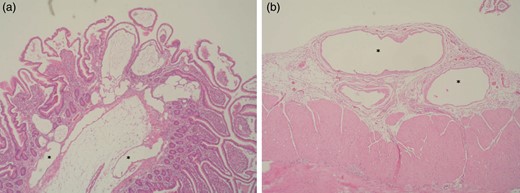
(a) Histopathology of the resected small intestine with dilated subserosal lymph vessels (*). (b) Histopathology of the resected small intestine with dilated submucosal lymph vessels (*).
The patient was discharged on the seventh postoperative day. During an outpatient visit after 2 weeks, a slight improvement of the total serum protein to 52 g/l was obtained.
An outpatient follow-up after 6 months showed a reduction in the patient's weight from 110 to 105 kg (BMI: 31 kg/m²), and the frequency of lymph drainage had been reduced to twice per week. Physical capabilities improved, and diarrhoea has not occurred since 4 weeks after the operation. Total serum protein level was at the lower end of the normal range (63 g/l) with an otherwise normal serum electrophoresis.
DISCUSSION
Taking PIL into account for a differential diagnosis in adults is a challenge for gastroenterologists, since PIL presents with varying symptoms [1, 4, 7]. In contrast to an intraoperatively diagnosed case of PIL [2], the current case was presented for surgical resection of an already diagnosed PIL.
The lymph fluid was lost intraluminally (diarrhoea) in the current case and extraluminally (chylous ascites) in our first case. This might be explained by the chronic lymphedema leading to dilation of the vessels and sometimes even to a rupture leading to a loss of lymph fluid into the peritoneal cavity [3].
Surgical resection of the affected intestine has been described as a possible treatment option in patients with a segmental intestinal lymphangiectasia if conservative treatment is unable to control the symptoms. Capsule endoscopy confirmed the limited extension of PIL and served as valuable preoperative tool. Although laparoscopic exploration can be used to examine the intestine intraoperatively, this can be limited to uncertain cases if capsule endoscopy is performed first. In adults, only five cases of PIL with surgical treatment have been described [2, 8–10] (Table 1). Three patients underwent elective surgery, whereas two presented with acute ileus and a gastrointestinal bleeding. The elective patients showed common symptoms of PIL and are asymptomatic after resection of the affected intestine. The current case is the first described laparoscopic resection of PIL in adults.
| Publication (year) . | Sex . | Age . | Symptoms . | Time until diagnosis . | Laboratory findings . | Imaging . | Imaging results . | Surgery . | Outcome (follow-up in moths) . |
|---|---|---|---|---|---|---|---|---|---|
| Lenzhofer [10] (1993) | Male | 26 | Ileus, epigastric pain of sudden onset and oedema of the extremities | Unknown | Severe hypoproteinaemia, low IgG concentration and lymphopenia | Conventional contrast radiography | Irregularly shaped nodular filling defect | Emergency conventional jejunal segment resection with a yellowish fist-sized deposit | Asymptomatic (14) |
| Chen [9] (2003) | Female | 49 | Epigastralgia and anaemia | ∼2 months | Low haemoglobin | Upper endoscopy | Irregular duodenal elevation of mucosa | Elective modified Whipple's operation with pylorus preservation | Asymptomatic (48) |
| Fang [8] (2007) | Female | 55 | Abdominal pain, oedema, diarrhoea | ∼20 years | Lymphopenia, albumin deficiency | CT, capsule endoscopy | Thickening of intestinal wall, dilation of lymphatic vessels and intestinal villi | Elective conventional resection of the affected small intestine | Unknown |
| Kneist [2] (2011) | Male | 58 | Therapy-refractory chylaskos, lower limb oedema | ∼30 years | General protein deficiency, hypocalcaemia | MRI with lymphography | Thickened intestinal wall, chylaskos | Elective conventional resection of 100 cm small intestine | Asymptomatic (9) |
| Maamer [4] (2012) | Male | 37 | Gastrointestinal bleeding, melanea | Unknown | Low haemoglobin | Chylous effusion with cystic formations | Emergency conventional 40 cm small bowel resection | Unknown | |
| Current case | Male | 51 | Lower limb oedema, diarrhoea, physical limitations | ∼20 years | General protein deficiency | Push–pull enteroscopy, capsule endoscopy | Thickening of intestinal mucosa, dilated lymph vessels | Elective laparoscopic resection of 95 cm altered small intestine | No diarrhoea, better physical capabilities, normal serum protein (6) |
| Publication (year) . | Sex . | Age . | Symptoms . | Time until diagnosis . | Laboratory findings . | Imaging . | Imaging results . | Surgery . | Outcome (follow-up in moths) . |
|---|---|---|---|---|---|---|---|---|---|
| Lenzhofer [10] (1993) | Male | 26 | Ileus, epigastric pain of sudden onset and oedema of the extremities | Unknown | Severe hypoproteinaemia, low IgG concentration and lymphopenia | Conventional contrast radiography | Irregularly shaped nodular filling defect | Emergency conventional jejunal segment resection with a yellowish fist-sized deposit | Asymptomatic (14) |
| Chen [9] (2003) | Female | 49 | Epigastralgia and anaemia | ∼2 months | Low haemoglobin | Upper endoscopy | Irregular duodenal elevation of mucosa | Elective modified Whipple's operation with pylorus preservation | Asymptomatic (48) |
| Fang [8] (2007) | Female | 55 | Abdominal pain, oedema, diarrhoea | ∼20 years | Lymphopenia, albumin deficiency | CT, capsule endoscopy | Thickening of intestinal wall, dilation of lymphatic vessels and intestinal villi | Elective conventional resection of the affected small intestine | Unknown |
| Kneist [2] (2011) | Male | 58 | Therapy-refractory chylaskos, lower limb oedema | ∼30 years | General protein deficiency, hypocalcaemia | MRI with lymphography | Thickened intestinal wall, chylaskos | Elective conventional resection of 100 cm small intestine | Asymptomatic (9) |
| Maamer [4] (2012) | Male | 37 | Gastrointestinal bleeding, melanea | Unknown | Low haemoglobin | Chylous effusion with cystic formations | Emergency conventional 40 cm small bowel resection | Unknown | |
| Current case | Male | 51 | Lower limb oedema, diarrhoea, physical limitations | ∼20 years | General protein deficiency | Push–pull enteroscopy, capsule endoscopy | Thickening of intestinal mucosa, dilated lymph vessels | Elective laparoscopic resection of 95 cm altered small intestine | No diarrhoea, better physical capabilities, normal serum protein (6) |
| Publication (year) . | Sex . | Age . | Symptoms . | Time until diagnosis . | Laboratory findings . | Imaging . | Imaging results . | Surgery . | Outcome (follow-up in moths) . |
|---|---|---|---|---|---|---|---|---|---|
| Lenzhofer [10] (1993) | Male | 26 | Ileus, epigastric pain of sudden onset and oedema of the extremities | Unknown | Severe hypoproteinaemia, low IgG concentration and lymphopenia | Conventional contrast radiography | Irregularly shaped nodular filling defect | Emergency conventional jejunal segment resection with a yellowish fist-sized deposit | Asymptomatic (14) |
| Chen [9] (2003) | Female | 49 | Epigastralgia and anaemia | ∼2 months | Low haemoglobin | Upper endoscopy | Irregular duodenal elevation of mucosa | Elective modified Whipple's operation with pylorus preservation | Asymptomatic (48) |
| Fang [8] (2007) | Female | 55 | Abdominal pain, oedema, diarrhoea | ∼20 years | Lymphopenia, albumin deficiency | CT, capsule endoscopy | Thickening of intestinal wall, dilation of lymphatic vessels and intestinal villi | Elective conventional resection of the affected small intestine | Unknown |
| Kneist [2] (2011) | Male | 58 | Therapy-refractory chylaskos, lower limb oedema | ∼30 years | General protein deficiency, hypocalcaemia | MRI with lymphography | Thickened intestinal wall, chylaskos | Elective conventional resection of 100 cm small intestine | Asymptomatic (9) |
| Maamer [4] (2012) | Male | 37 | Gastrointestinal bleeding, melanea | Unknown | Low haemoglobin | Chylous effusion with cystic formations | Emergency conventional 40 cm small bowel resection | Unknown | |
| Current case | Male | 51 | Lower limb oedema, diarrhoea, physical limitations | ∼20 years | General protein deficiency | Push–pull enteroscopy, capsule endoscopy | Thickening of intestinal mucosa, dilated lymph vessels | Elective laparoscopic resection of 95 cm altered small intestine | No diarrhoea, better physical capabilities, normal serum protein (6) |
| Publication (year) . | Sex . | Age . | Symptoms . | Time until diagnosis . | Laboratory findings . | Imaging . | Imaging results . | Surgery . | Outcome (follow-up in moths) . |
|---|---|---|---|---|---|---|---|---|---|
| Lenzhofer [10] (1993) | Male | 26 | Ileus, epigastric pain of sudden onset and oedema of the extremities | Unknown | Severe hypoproteinaemia, low IgG concentration and lymphopenia | Conventional contrast radiography | Irregularly shaped nodular filling defect | Emergency conventional jejunal segment resection with a yellowish fist-sized deposit | Asymptomatic (14) |
| Chen [9] (2003) | Female | 49 | Epigastralgia and anaemia | ∼2 months | Low haemoglobin | Upper endoscopy | Irregular duodenal elevation of mucosa | Elective modified Whipple's operation with pylorus preservation | Asymptomatic (48) |
| Fang [8] (2007) | Female | 55 | Abdominal pain, oedema, diarrhoea | ∼20 years | Lymphopenia, albumin deficiency | CT, capsule endoscopy | Thickening of intestinal wall, dilation of lymphatic vessels and intestinal villi | Elective conventional resection of the affected small intestine | Unknown |
| Kneist [2] (2011) | Male | 58 | Therapy-refractory chylaskos, lower limb oedema | ∼30 years | General protein deficiency, hypocalcaemia | MRI with lymphography | Thickened intestinal wall, chylaskos | Elective conventional resection of 100 cm small intestine | Asymptomatic (9) |
| Maamer [4] (2012) | Male | 37 | Gastrointestinal bleeding, melanea | Unknown | Low haemoglobin | Chylous effusion with cystic formations | Emergency conventional 40 cm small bowel resection | Unknown | |
| Current case | Male | 51 | Lower limb oedema, diarrhoea, physical limitations | ∼20 years | General protein deficiency | Push–pull enteroscopy, capsule endoscopy | Thickening of intestinal mucosa, dilated lymph vessels | Elective laparoscopic resection of 95 cm altered small intestine | No diarrhoea, better physical capabilities, normal serum protein (6) |
In conclusion, intestinal lymphangiectasia is a possible differential diagnosis of a chronic protein deficiency and should be taken into consideration. Resection of the altered intestine is a possible treatment option in symptomatic and therapy-refractory cases. Whether surgical resection is the treatment of choice and may be considered earlier in the treatment process could be part of future investigations.
SUPPLEMENTARY MATERIAL
Supplementary material is available at the Journal of Surgical Case Reports online.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- lymphedema
- diarrhea
- diet
- enteroscopy
- adult
- chylous ascites
- differential diagnosis
- dilatation, pathologic
- intestines
- laparoscopy
- intestinal lymphangiectasis
- rupture
- surgical procedures, operative
- peritoneum
- somatostatin
- clinical diagnostic instrument
- lymphedema, chronic
- capsule endoscopy
- excision
- conservative treatment
- rare diseases



