-
PDF
- Split View
-
Views
-
Cite
Cite
Selam Yekta Sendul, Cemile Ucgul, Fevziye Kabukcuoglu, Burcu Dirim, Dilek Guven, Primary orbital Ewing's sarcoma presenting with local recurrence to maxillary sinus shortly after tumor resection, Journal of Surgical Case Reports, Volume 2015, Issue 7, July 2015, rjv070, https://doi.org/10.1093/jscr/rjv070
Close - Share Icon Share
Abstract
Ewing's sarcoma (ES) is a malignant, small-round-cell neoplasm that normally affects the long bones of the limbs or the pelvis. Primary orbital ES of the skull has been considered extremely rare. We describe the case of a 19-year-old female patient with primary ES originating from the inferior orbital rime and, shortly after tumor resection, local recurrence to the maxillary sinus.
INTRODUCTION
Ewing's sarcoma (ES) is a malignant tumor that was first described as an endothelioma of bone by James Ewing in 1921 [1]. It typically occurs in primary long bones during the first and the second decades of life and rarely in the orbit of the skull [2]. Primary ES of the head and neck region is unusual and generally involves the mandible or the maxilla [3]. It has classically been studied under the heading of small, round-cell neoplasms of neuroectodermal origin [3]. Since ES is difficult to control, early diagnosis is crucial and the treatment requires a multimodality approach constituting chemotherapy, surgery and radiotherapy.
In this case, we focused on the clinicoradiological presentation and management principles of this rare manifestation of the primary orbital ES with local recurrence to the maxillary sinus shortly after the first resection. The study was conducted in accordance with the tenets of the Declaration of Helsinki by obtaining written consent from patient, with the approval of the local ethical review board.
CASE REPORT
A 19-year-old female patient visited our clinic with complaints of a painless mass in the inferior eye lid of the right eye (OD). Best-corrected visual acuity was measured 10/10 with a Snellen card in both eyes. On palpation, a firm, irregular, non-reducible mass of ∼3 cm was noted in the inferior orbital rim of the OD (Fig. 1a). The mass was inseparable from the inferior orbital rim. Additionally, there was diplopia on the downward gaze and ophthalmoparesis in the OD. Fundus examination of both eyes was normal. The patient's history and general physical examination were unremarkable. A complete blood cell count and serum laboratory values were normal. Magnetic resonance imaging (MRI) revealed an extraconal solid mass measuring 3 × 3 cm in the region of the right inferior temporal orbital wall (Fig. 1b). The paranasal sinuses were normal. No definite intracranial extension was seen.
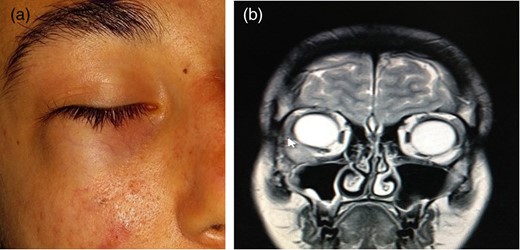
(a) A 19-year-old female patient with an immobile mass in the right inferior temporal location. (b) The MRI results of the patient show a mass fixed to the inferior orbital wall.
Anterior transconjunctival orbitotomy was performed for excisional biopsy and the removal of the tumor with its periosteum due to the erosion of the inferior orbital wall. The resected tumor was 3 × 3 × 3 cm and the tumor had caused lytic lesions on the inferior orbital wall. The tumor tissues resected in the surgery were fixed in 10% formalin, embedded in paraffin and then processed for light microscopy. The tissue sections were stained with hematoxylin and eosin (H&E), and examined immunohistochemically. After the surgery, the patient's diplopia with right and inferior ophthalmoparesis disappeared. At postoperative week 3, while we were waiting for the pathological diagnosis of the resected tumor, the patient visited our clinic with complaints of anesthesia and fullness on her right cheek. There was paresthesia in the region where the right infraorbital nerve innerved. Control MRI revealed a mass that invaded the anterolateral wall of the right maxillary sinus (Fig. 2a and b). In the meantime, tumor cells were positive in the membranous pattern for CD99 immunostaining and Periodic acid—Schiff (PAS) (Fig. 3a–c).
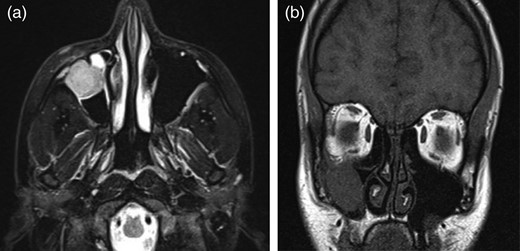
(a and b) The emergency MRI results of the patient who had complaints of infraorbital anesthesia in the postoperative week 3 revealed a mass invading the right maxillary sinus and probably compressing on the infraorbital nerve.
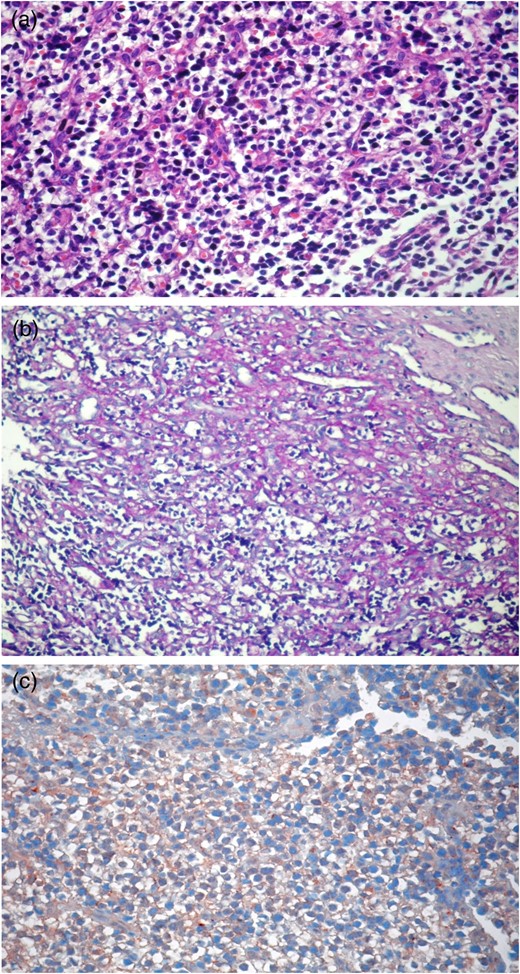
(a–c) Round-shaped, narrow eosinophilic cytoplasm cells with hyperchromatic nuclei (b: PAS+ and c: CD99+).
According to the results of further metastatic evaluation including PET–computed tomography and Technetium-99 whole-body bone scintigraphy, we did not detect any other tumor regions. In consequence of these examinations, we considered this tumor as primary orbital ES. We referred the patient to our oncology department. A chemotherapy treatment protocol of six cycles with Vincristine, Doxorubicin, Cyclophosphamide and Mesna was organized by the oncology clinic. In the control examination after the first cycle, it was observed that the complaints of anesthesia and parasthesia recovered.
DISCUSSION
In 1921, Ewing [1] first reported that an endothelioma of bone, which is the tumor known as ES, commonly arises from long bones and is more common in men and children under the age of 18 years. It belongs to the family of primitive neuroectodermal tumors, which are poorly differentiated neoplasms believed to be of neural crest origin. Primary ES in the head and neck regions constitute <4% of all ES [3]. Primary ES in the orbit is extremely rare and usually metastasizes [4, 5]. Ophthalmoplegia, proptosis and loss of vision due to primary orbital ES have been reported [4, 5].
The majority of primary ES of paranasal sinuses develops from the maxillary sinus [6–8]. In most instances, the tumor has local extension to the maxillary sinus, frontal sinus, nasal septum, nasal cavity, orbit, base of skull or a combination of the above. There was only one case where the tumor was isolated to the sphenoid sinus [3], and three cases where tumors were limited within the nasal cavity [9, 10]. Comparatively, patients with ethmoid sinus ES seemed to have a higher propensity for local extension of the tumor into the orbit and the cranium. This is likely due to the limited sinus space of the ethmoid sinus resulting in direct invasion of the tumor into the surrounding structures either through the thin bony lamina papyracea into the orbit or through the skull base into the cranium. On the other hand, the maxillary sinus has a larger sinus space and much thicker infraorbital bone making these expansions less likely [2].
In our patient, local invasion from the right orbit to the right maxillary sinus was observed 3 weeks after the tumor resection. We were surprised with this local recurrence in a very short time. We thought that since we removed the periosteum of the inferior orbital wall, we facilitated the local invasion of the tumor to the maxillary sinus. We did not plan a second operation. The patient is still receiving treatment in the oncology department.
To our knowledge, our patient is the first patient in whom the primary orbital ES invaded the maxillary sinus 3 weeks after the primary tumor resection.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
Thanks are due to Ayse Unal Ersonmez and Barbara Reid for editing the paper in terms of English.



