-
PDF
- Split View
-
Views
-
Cite
Cite
Henrietta Creasy, Luke Meleagros, Excess anticoagulation as a cause of small-bowel obstruction: a report of two cases, Journal of Surgical Case Reports, Volume 2015, Issue 4, April 2015, rjv041, https://doi.org/10.1093/jscr/rjv041
Close - Share Icon Share
Abstract
Spontaneous intramural haemorrhage is a rare cause of small-bowel obstruction, occurring most commonly in those who are anticoagulated. We describe two cases that presented with a history and imaging suggestive of small-bowel obstruction; both had International Normalized Ratios of above 10 on admission. The first case, a 62-year-old lady on warfarin for atrial fibrillation, was managed conservatively with good effect. In contrast, the second case, a 57-year-old gentleman on warfarin for his metallic aortic valve, underwent diagnostic laparotomy that revealed a 30-cm segment of proximal jejunum with spontaneous intramural haemorrhage. In this study, we emphasize the merit of conservative management for this rare cause of small-bowel obstruction.
INTRODUCTION
For those patients presenting with symptoms of small-bowel obstruction, the list of differential diagnoses is vast, with numerous extramural, mural and luminal causes. In this report, we describe two cases that presented with a history and imaging suggestive of small-bowel obstruction. Both had deranged clotting function as a result of excess anticoagulation. We present their subsequent management and emphasize the merit of conservative management for this rare cause of small-bowel obstruction.
CASE REPORT
Case 1
The first case we report is of a 62-year-old lady with a background of atrial fibrillation, hypertension and chronic obstructive pulmonary disease, who presented with a 2-day history of abdominal pain, distension and vomiting of bilious fluid. She had not passed stools or flatus.
On examination she appeared uncomfortable, with an irregular pulse rate of 144, but she was maintaining her blood pressure at 116/70 mmHg. On palpation, her abdomen was distended with generalized tenderness; she was maximally tender in the left iliac fossa. Per rectal examination revealed soft stool in the rectum, no masses or blood.
Laboratory investigations revealed an International Normalized Ratio (INR) of 10; she was anticoagulated with warfarin due to her atrial fibrillation. Initial imaging revealed dilated small-bowel loops on abdominal radiograph (Fig. 1).

Abdominal radiograph showing dilated small-bowel loops (Case 1).
A CT scan was performed that showed dilation of the proximal small bowel, with a long segment of thickened small-bowel loops that was reported as possible intussusception (Fig. 2). The images were discussed further at the multidisciplinary surgical radiology meeting in the context of her haematology results. It was determined that the long segment of the thickened small bowel was, in fact, haemorrhage rather than intussusception.
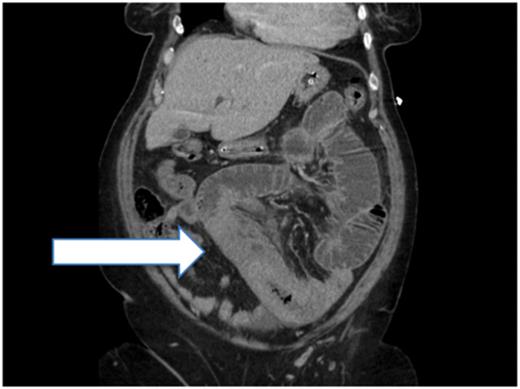
Post-contrast CT (sagittal plane) showing proximal small-bowel dilation and a thickened small-bowel segment (Case 1).
The patient was managed conservatively with intravenous fluids, a nasogastric tube and bowel rest. Her warfarin was withheld and her anticoagulation was reversed with fresh frozen plasma and vitamin K over the course of 4 days. She improved clinically and tolerated oral intake with the passage of stool. A small-bowel meal 4 days after admission revealed no residual evidence of obstruction and she was discharged home.
Case 2
The second case described is of a 57-year-old gentleman who presented with a 3-day history of abdominal pain, vomiting and absolute constipation. His past medical history of note was a metallic aortic valve, although he was unable to give an accurate drug history on admission. On examination, his abdomen was distended with generalized abdominal tenderness and sluggish bowel sounds. Abdominal radiograph revealed dilated small-bowel loops (Fig. 3), and he was managed as a case of small-bowel obstruction, with intravenous fluid and a nasogastric tube.

Abdominal radiograph showing dilated small-bowel loops (Case 2).
The following morning on the post-take ward round he was peritonitic and a decision was made to take him for an exploratory laparotomy prior to further imaging. An INR was sent as a work-up for theatre, which returned at 12.6; drug reconciliation revealed that he was on warfarin. Berriplex was used to normalize his clotting prior to theatre on advice from haematology.
Intraoperatively, there was a 30-cm segment of proximal jejunum with spontaneous intramural haemorrhage; the bowel was viable with pulsatile vessels in the mesentery. There was no intraluminal bleeding or any other cause for obstruction; therefore, washout and closure was performed without resection. Postoperatively, he recovered well and was discharged on Clexane, with the view to restarting warfarin in the community.
DISCUSSION
Spontaneous intramural haemorrhage is characterized by bleeding into the submucosal layer of the bowel in the absence of trauma. The jejunum is the most commonly affected site, followed by the ileum and then duodenum [1]. This is in contrast to traumatic intramural haemorrhage primarily seen in the duodenum due to its retroperitoneal components. It occurs during a hypercoagulable state, excess anticoagulation due to warfarin therapy being the most frequent aetiology, but case reports also describe such a presentation in those with haemophilia, haematological malignancies and chemotherapy treatment [2]. The symptoms are indistinguishable from other causes of small-bowel obstruction, although there may be a history of warfarin therapy or peripheral stigmata of excess anticoagulation.
Clotting may be grossly deranged, with INRs of over 10 commonly seen. A contrast CT scan of the abdomen and pelvis is the imaging modality of choice, classically showing circumferential hyperdensity and wall thickening, with luminal narrowing and obstruction.
The management of small-bowel obstruction secondary to intramural haemorrhage is predominantly conservative, including reversal of clotting factors. Operative management may be indicated if diagnostic uncertainty remains or there is haemodynamic instability due to active bleeding [3]. Abbas et al. presented data from 13 cases of spontaneous intramural small-bowel haemorrhage, retrospectively analysed with regard to inpatient outcomes and long-term morbidity. Eleven of the 13 patients were managed conservatively with no significant sequelae at a mean follow-up of 35 months; the two patients who underwent laparotomy had a viable small bowel and no resections were undertaken [4].
In an aging population, with a large number of patients anticoagulated for medical conditions such as atrial fibrillation, spontaneous intramural haemorrhage is a differential that must be considered. Identification of hyperdense intramural bleeding, in the context of grossly deranged clotting, may avoid the morbidity of undergoing a potentially unnecessary laparotomy.
CONFLICT OF INTEREST STATEMENT
None declared.



