-
PDF
- Split View
-
Views
-
Cite
Cite
Jordyn Vernon, Colin Schieman, Laura Schneider, Waël C. Hanna, Rare case of subcarinal thymic carcinoma in the middle mediastinum, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv030, https://doi.org/10.1093/jscr/rjv030
Close - Share Icon Share
Abstract
We report an extremely rare case of a thymic carcinoma occurring in the subcarinal location of the middle mediastinum, masquerading as subcarinal adenopathy. A 6.2 × 5 cm mass was detected on computed tomography scan and found to be hypermetabolic on positron emission tomography scan. Transbronchial biopsy was performed and the mass was found to be suspicious for malignancy. A thoracoscopic resection of the mass was performed and found to be thymic carcinoma. The patient underwent a course of adjuvant radiation. To the best of our knowledge, this is the first reported case of a thymic carcinoma resected from the middle mediastinum.
INTRODUCTION
Thymic neoplasms account for ∼20% of all mediastinal tumors [1]. Malignant thymic neoplasms can be broadly divided into thymomas and thymic carcinomas, both of which exist almost exclusively in the anterior mediastinum [1]. Thymomas have also been described in the neck, posterior mediastinum, lungs, base of the skull and pleural cavity [2–5]. Very few case reports have described thymomas occurring in the middle mediastinum [2–5]. Unlike thymomas, thymic carcinomas have only been observed in the anterior mediastinum. To our knowledge, this report will describe the first case of thymic carcinoma in the middle mediastinum.
CASE REPORT
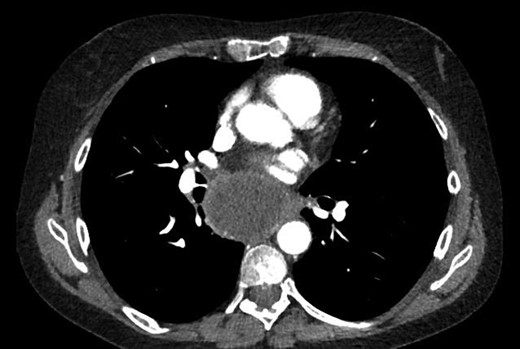
A 55-year-old Caucasian female presented with productive cough, dyspnea, chest pain and weight loss. The patient's medical history was significant for hypertension, hypercholesterolemia, dyslipidemia, chronic renal failure, gastroesophageal reflux disease and chronic anemia. She was a 30 pack-year smoker and her mother was diagnosed with lung cancer. Her physical examination was unremarkable. An initial chest X-ray showed a large subcarinal mass. On computed tomography (CT), a 6.2 × 5 cm tumor was detected in the subcarinal area (Figs 1 and 2). A bronchoscopy with transbronchial biopsy was performed, and the resulting pathological analysis was suspicious for malignant cells; however, no specific tumor type was identified. A positron emission tomography scan showed a large hypermetabolic subcarinal lesion with a standard uptake value of 14.3, consistent with malignancy. The differential diagnosis at the time included an infected bronchogenic cyst, esophageal duplication cyst or a malignant subcarinal lymph node. Thoracoscopic surgical resection was planned for diagnostic and therapeutic purposes.
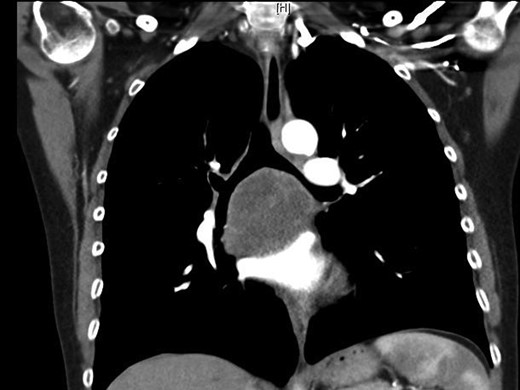
Subcarinal tumor on preoperative CT of the chest, coronal cuts.
Prior to surgical resection, esophagoscopy and bronchoscopy documented the absence of any communication of this mass to the esophagus and airway. The resection was completed thoracoscopically, with a five-port approach. One port was made at the mid-axillary line of the eighth intercostal space for the camera, in addition to two anterior and two posterior ports. The dissection of the tumor began at the level of the inferior pulmonary ligament and posterior mediastinum, all the way to the azygous vein. The esophagus was found completely adherent to the tumor, necessitating an esophageal myotomy for en bloc resection. The esophageal mucosa was not violated at any point throughout the procedure. The anterior dissection proceeded at the level of the posterior atrial wall, the inferior and superior pulmonary veins, the main trunk of the pulmonary artery, and the membranous areas of the right and left main stem bronchi. Complete gross resection was observed at the conclusion of the operation. At the end of the procedure, intraoperative endoscopy was performed to evaluate the esophageal wall. Air was insufflated into the esophagus to confirm the absence of any leaking from the mucosa.
The specimen consisted of an encapsulated red-brown tissue weighing 57 g, and measuring 5.5 × 4.5 × 5 cm. The mass was largely necrotic and surrounded by fibrous tissue. Some sheets of viable tumor cells were present, and these contained pleomorphic nuclei, vesicular chromatin, and prominent nucleoli. The tumor cells were strongly positive for CAM 5.2, but negative for CK7, CK5/6, CK19, Calretinin, TTF1, CEA, AFP, HCG, PLAP, CD5 and CD56. This excluded any cells of pulmonary, mesothelial or germ cell origin. Thus, thymic carcinoma was determined to be the most fitting diagnosis based on the morphology and staining. The surgical margins were clear of malignant cells.
The patient was referred for adjuvant radiation. At the most recent follow-up visit 9 months after surgery, the patient was well with no evidence of recurrence on CT scan.
DISCUSSION
Thymic carcinomas are rare and account for only 1% of all thymic neoplasms [1]. All thymic carcinomas reported to date have been located in the anterior compartment of the mediastinum [1]. To the best of our knowledge, this is the first case report of a thymic carcinoma occurring in the middle mediastinum. The differential diagnosis of middle mediastinal tumors usually includes bronchogenic cysts, enterogenous cysts, neuroenteric cysts, pericardial cysts and lymphangiomas [1]. Very selected cases of thymoma have been reported in the middle mediastinum [2–5]. These are attributed to the presence of ectopic thymic tissue in the subcarinal area due to failure of the thymus to migrate into the anterosuperior mediastinum during embryological development [2–5]. By way of the same process, it is therefore theoretically possible for these cells to undergo malignant degeneration into thymic carcinoma, although this has not been previously described.
When compared with thymomas, thymic carcinomas have considerably worse prognosis [1]. When possible, complete surgical resection is the treatment of choice for thymic carcinomas [1, 6]. Therefore, when planning surgical resection, it is important to consider malignant neoplasms as part of the differential diagnosis of middle mediastinal tumors. Although rare, thymic carcinomas and other malignant tumors of the middle mediastinum should be resected with negative margins, in order to decrease the risk of local recurrence and improve prognosis.
This is the first case report of a malignant thymic carcinoma occurring in the middle mediastinum at the subcarinal location. This pathology, although rare, should be added to the differential diagnosis of middle mediastinal tumors. When planning surgical resection of such tumors, complete excision with negative margins should be attempted to minimize chances of local recurrence and improve prognosis.
CONFLICT OF INTEREST STATEMENT
None declared.



