-
PDF
- Split View
-
Views
-
Cite
Cite
Sala Abdalla, Peter Macneal, Cynthia-Michelle Borg, Metastases of lobular breast carcinoma in the terminal ileum and ileocaecal valve, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv028, https://doi.org/10.1093/jscr/rjv028
Close - Share Icon Share
Abstract
Gastrointestinal (GI) metastases from primary breast carcinoma are rare but more common in invasive lobular carcinoma than invasive ductal carcinoma. The symptoms may be non-specific and the presentation can occur many years after the initial primary breast carcinoma. Radiological and endoscopic findings can be difficult to distinguish from inflammatory bowel disease and primary carcinoma of the GI tract. Histological and immunohistopathology assessment will usually confirm the diagnosis of metastatic breast carcinoma. We report the first case of lobular breast carcinoma metastasizing to the terminal ileum and ileocaecal valve 19 years following treatment for breast cancer in an 82-year-old woman. Staging investigations revealed synchronous metastases in bones and the pleura. A high index of suspicion and awareness of the potential long interval in the presentation of metastatic breast cancer help in making an accurate diagnosis and rapid clinical management.
INTRODUCTION
Metastases of breast carcinoma are commonly found in the bone, liver, lungs and the brain. Gastrointestinal (GI) involvement is rare, with only few cases of such metastases reported in the literature [1]. Invasive lobular carcinoma (ILC) accounts for 5–10% of invasive breast carcinomas. Of the various histological subtypes it is more commonly associated with metastases to the peritoneum, ovaries, uterus and GI tract [2]. Although rare, colorectal metastases of ILC of the breast are a diagnostic challenge since they can simulate primary colon cancer or inflammatory bowel disease. Often there may be a long disease-free interval and diagnosis therefore requires a high index of clinical suspicion.
Here we report a case of metastases of lobular breast carcinoma in the terminal ileum (TI) and ileocaecal valve (ICV), associated with synchronous metastases to bones and the pleura, 19 years following treatment for primary breast carcinoma.
CASE REPORT
An 82-year-old female presented to the Emergency Department with a 48 h history of colicky central abdominal pain associated with vomiting and loose stools. There was no report of rectal bleeding. She also gave a 2 months' history of unintentional weight loss of 12 kg. She had a history of right breast ILC (T3N1M0) which was treated 19 year previously with a modified radical mastectomy, axillary node clearance and adjuvant chemotherapy. The tumour had been oestrogen receptor (ER) and progesterone receptor (PR) positive and she had completed 5 years of adjuvant Tamoxifen. Seven out of 29 lymph nodes were positive for metastatic disease. Her other medical history included hypertension and hypercholestrolaemia.
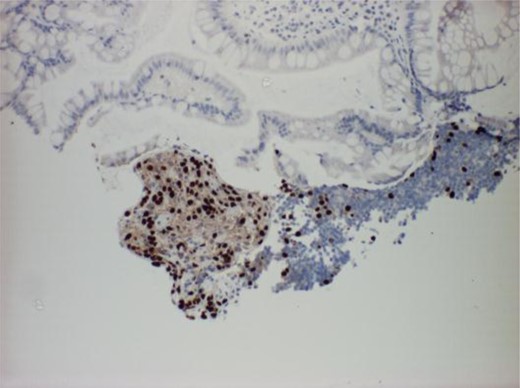
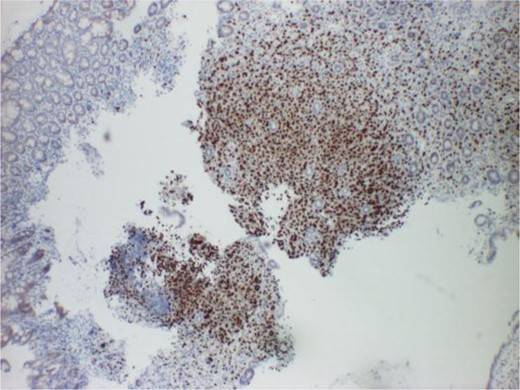
The physical examination revealed central abdominal tenderness with no palpable masses and no peritonism. Laboratory tests showed a mild normocytic anaemia (haemoglobin count 11.2 g/dl) and an elevated erythrocyte sedimentation rate count of 108. Computed tomography (CT) scanning revealed thickening of the wall of the caecum and suspicious lesions in the vertebrae and iliac bones. A follow-up colonoscopy reported inflammation around the proximal caecal folds, ICV and TI (Fig. 1). Biopsies from the TI and ICV confirmed adenocarcinoma with an infiltrative pattern being consistent with metastatic lobular carcinoma of the breast (Figs 2–4). This was further evaluated by immunohistopathology as demonstrating expression of ER and Cytokeratin 7 (CK7) but negative for CK20 and E-cadherin. Biopsies from the ascending transverse and sigmoid colon were negative for malignancy. Findings from a subsequent staging CT scan showed a right basal pleural effusion, which upon cytological analysis was confirmed as metastatic lobular carcinoma. Nuclear medicine bone scans revealed extensive bone metastases involving the whole spine, skull, ribs, humeri and femur bones. There was no evidence of recurrence in remaining breast or chest wall.
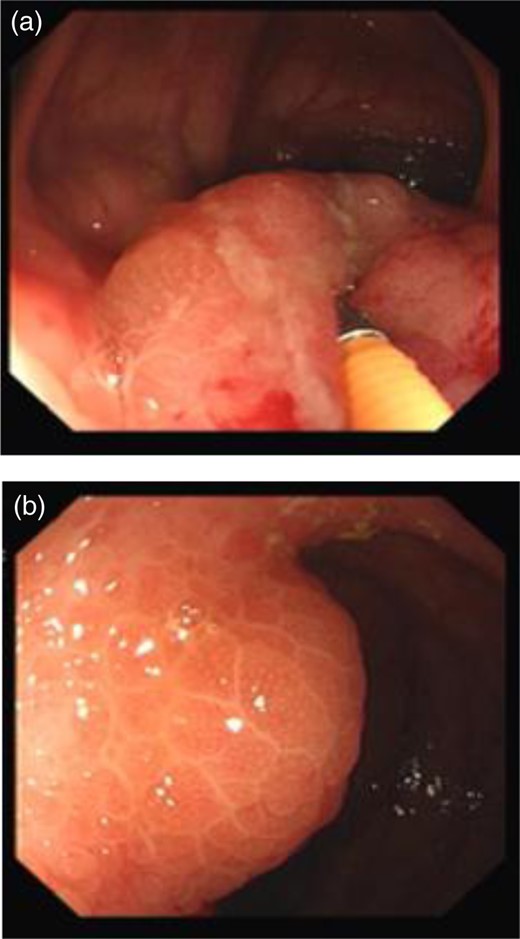
Colonoscopy views showing inflammation in the ICV (a) and TI (b).
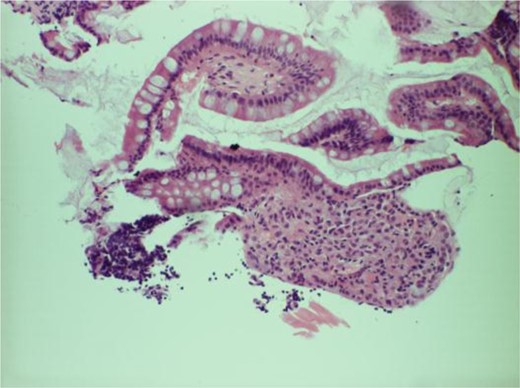
Histology slide of tissue from the ICV showing deposits of lobular breast carcinoma and infiltration of neutrophils into the surface epithelium and lamina propria.
She was started on palliative hormonal therapy (letrozole) and denosumab with planned regular follow-up with the medical oncologists.
DISCUSSION
GI metastases from breast cancer are rare and can occur many years after the primary cancer. Borst and Ingold [3] in their study of 2604 cases of breast cancer over an 18-year period reported GI metastases in only 17 cases (0.7%). A review of 12 001 cases by McLemore et al. [4] showed that GI metastases from primary breast carcinoma were as rare as 73 cases, with a mean interval from diagnosis of 7 years. However, breast cancer is the second most common malignancy to metastasize to the GI tract, after malignant melanoma [5]. GI metastases occur more commonly in ILC than invasive ductal carcinoma and the reason for the variation in this metastatic pattern is not well understood. Among GI metastases the most commonly afflicted sites are the stomach and small intestine, with comparably fewer reports of dissemination to the colon and rectum [6].
Our case study is the first to report metastases from ILC to the TI and ICV with synchronous involvement of bones and the pleura. The bony metastases and malignant pleural effusion were discovered incidentally during staging investigations. The patient had had no related symptoms.
Symptoms of metastatic disease to the GI tract may be non-specific. Our patient had presented with a short history of GI symptoms which could have suggested gastroenteritis as a likely diagnosis. The 19-year interval between the primary diagnosis of breast cancer and occurrence of metastases would have made the diagnosis of bowel metastases unusual. Schwarz et al. [7] reported a median interval between breast cancer and the GI metastases of 6 years (range 0.25–12.5 years) and McLemore et al. [4] found a median interval of 7 years. Our case demonstrates one of the longest time intervals between primary and GI metastatic disease reported in the literature. Furthermore, the inflammation around the TI during endoscopy made it difficult to differentiate its macroscopic appearance from inflammatory bowel disease. Colorectal metastases from lobular breast carcinoma can demonstrate nodular and cobblestone-like thickening of the mucosa that can mimic Crohn's disease [8]. Additionally, metastatic lesions involving the colon may be difficult to differentiate from primary malignancies at these sites.
Diagnosis of GI metastases in the context of present or previous breast cancer primarily requires a high degree of suspicion, particularly in patients with a history of lobular breast carcinoma. Endoscopic evaluation with tissue sampling for histological assessment will provide the final diagnosis that can be confirmed with immunohistopathology analysis.
Due to the relatively small number of reported cases, there remains a paucity of guidelines for managing such presentations. Treatment usually comprises chemotherapy, endocrine therapy or both combined; with remission being reported in 32–58% of patients [9]. While palliative surgery was not shown to result in an increased overall survival [4], surgical intervention may be reserved for emergency presentations of perforation or haemorrhage in selected isolated lesions [10]. Overall survival after diagnosis of GI metastases from a breast primary is poor with few patients surviving beyond 2 years, although reports of survival of up to 9 years have been published [6]. It therefore follows that any unusual GI symptoms present in a patient with a history of lobular carcinoma of the breast should be treated with a high index of suspicion.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
CONFLICT OF INTEREST STATEMENT
None declared.



