-
PDF
- Split View
-
Views
-
Cite
Cite
Kristin Long, Tessa Cartwright, David Sloan, Cortney Lee, Cystic multiglandular maternal hyperparathyroidism diagnosed by neonatal hypocalcemic seizures, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv031, https://doi.org/10.1093/jscr/rjv031
Close - Share Icon Share
Abstract
A 7-day-old male infant born to a healthy 33-year-old female at 37 weeks of gestation was brought to the local emergency department (ED) with sudden-onset tonic–clonic seizures. Laboratory testing revealed extreme hypocalcemia (ionized calcium of 3.2 mg/dl) and undetectable parathyroid hormone (PTH <10 pg/ml). Concomitant evaluation of the mother revealed both elevated ionized calcium (5.9 mg/dl) and PTH (116 pg/ml). The mother underwent preoperative ultrasound localization and sestamibi scan, followed promptly by parathyroidectomy. Given the cystic appearance and presence of multiglandular disease, evaluation for familial cystic parathyroid adenomatosis (hyperparathyroidism-jaw bone-tumor syndrome) and MEN 1 were undertaken. The infant was stabilized and discharged home. He returned to the ED with seizures at 1 month of age. After increasing calcium supplementation appropriately, he was monitored with weekly office visits. This represents a unique case of undiagnosed maternal primary hyperparathyroidism manifesting with intrauterine parathyroid suppression and hypocalcemic seizures in the newborn.
INTRODUCTION
Primary hyperparathyroidism is the most common cause of hypercalcemia in the outpatient setting. The occurrence during pregnancy is a rare event. The incidence in pregnant reproductive age women is reported to be 8 patients per 100 000 per year [1]. The most common cause of primary hyperparathyroidism in pregnancy, as in the general population, is a single adenoma [2].
In 1938, Friedrichsen described symptomatic hypocalcemia in an infant unmasking the mother's hyperparathyroidism [3]. Since this initial anecdotal publication, there have been fewer than 20 published cases of similar presentations of neonatal hypocalcemia leading to a diagnosis of maternal hyperparathyroidism.
Neonatal hypocalcemia, while fortunately rare, can be physiologic in origin and generally resolves shortly after birth. Late-onset or symptomatic hypocalcemia, however, can cause seizures in infants and warrants investigation of both the child and the mother. During the third trimester of pregnancy, calcium is actively transferred from the mother to the fetus [4]. Parathyroid hormone (PTH) and calcitonin, on the other hand, do not cross the placental barrier and serum calcium of a neonate is often higher than that of the mother at birth [5]. After birth, serum calcium regulation of the child is no longer dependent on the mother. Within the first 48 h, essentially all healthy newborns have a transient period of hypocalcemia. This is a normal transition phase due to the new dependence on their own immature PTH secretion, limited dietary calcium intake, immature renal reabsorption, minimal skeletal calcium stores and vitamin D status [6]. Other causes of hypocalcemia are abnormalities of vitamin D metabolism, hyperphosphatemia, hypomagnesemia and hypercalcitonemia, which typically occur within 12–24 h of life [5]. Hypocalcemia can result in convulsions, arrythmias, tetany and/or paresthesias in the hands, feet and perioral regions. Additionally, hypocalcemia may result in petechiae, hyperactive reflexes, prolonged QT waves and laryngospasms [6].
While most patients with hyperparathyroidism are diagnosed outside of pregnancy, neonatal manifestations of hypocalcemia can be a rare initial presentation of maternal hyperparathyroidism. Here, we present a case of a female with multiglandular hyperparathyroidism diagnosed only after her newborn child presented with seizures due to severe hypocalcemia.
CASE REPORT
A 7-day-old male infant born to a healthy 33-year-old female at 37 weeks of gestation presented to the local emergency department (ED) with sudden-onset tonic–clonic seizures. He was healthy at birth, with no prenatal complications, and was stable at discharge following birth. After intubation and treatment with anti-epileptic medication, a thorough investigation commenced. Laboratory testing revealed extreme hypocalcemia (ionized calcium of 3.2 mg/dl) and undetectable PTH (<10 pg/ml). Concomitant evaluation of the mother revealed both elevated ionized calcium (5.9 mg/dl) and PTH (116 pg/ml). Upon further review, the mother reported a history dating back several years with vague symptoms of constipation, labile mood and fatigue during and prior to her pregnancy. She had two other children, born healthy and from uncomplicated pregnancies. She denied any history of bone pain, kidney stones or abdominal pain, and denied any family history of calcium disorders.
With a diagnosis of primary hyperparathyroidism, the mother then underwent preoperative ultrasound localization and sestamibi scan. In-office ultrasound revealed an essentially normal thyroid with only a small subcentimeter nodule in the right inferior pole. Evaluation of the surrounding tissue for parathyroid abnormalities revealed a large 2- to 3-cm, hypodense area inferior to the right inferior thyroid pole. This area lacked blood flow but was not classic for parathyroid adenoma due to the almost anechoic appearance. Evaluation of the left side of the neck revealed similar hypodense changes in the lower neck but nothing as significant as seen on the right. A parathyroid nuclear scan was performed showing two sites of sestamibi hyperconcentration, slow washout and discordance in the left neck.
The patient was diagnosed with primary hyperparathyroidism likely due to multiglandular disease and was prepared for parathyroidectomy. After an extensive exploration, three significantly enlarged cystic glands were identified and removed (Fig. 1). Intraoperative PTH levels dropped appropriately after parathyroidectomy, thyroid lobectomy and cervical thymectomy from a baseline of 104 pg/ml to a final value of 41.1 pg/ml. Pathology noted three hypercellular, cystic parathyroid glands with mucoid degeneration weighing 6.200, 1.846 and 0.110 g as well as a separate 3 mm focus of hypercellular parathyroid tissue in the pretracheal tissue. The calcium the morning after surgery was normal at 8.7 mg/dl.
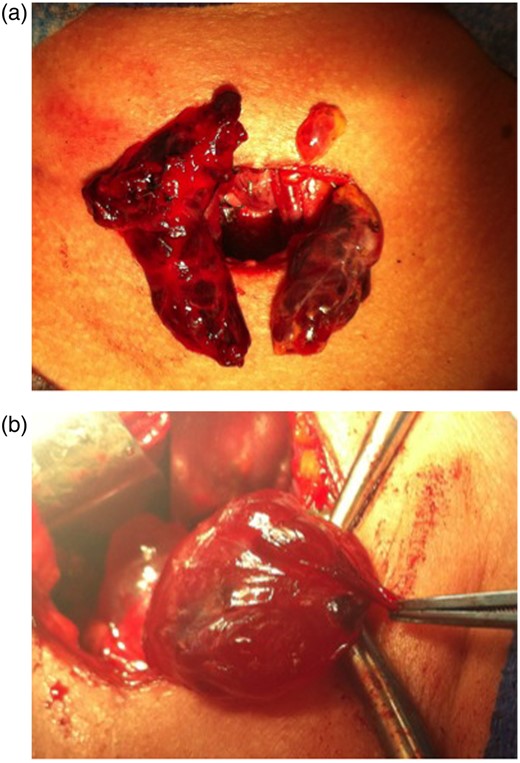
(a) Intraoperative photograph showing cystic parathyroid glands. (b) Cystic parathyroid glands.
Given the cystic appearance, age of the patient and presence of multiglandular disease, evaluation for familial cystic parathyroid adenomatosis (hyperparathyroidism-jaw bone-tumor syndrome) and MEN 1 were undertaken, both of which were normal. The infant was stabilized and discharged home. He returned to the ED with seizures at 1 month of age. After increasing calcium supplementation appropriately, he was monitored with weekly office visits. His medications were weaned slowly and discontinued at 9 months of age. He has since been maturing well with no further seizure activity and normal calcium levels. The mother also remains eucalcemic with a normal PTH. This represents a unique case of undiagnosed maternal primary hyperparathyroidism manifesting with intrauterine parathyroid suppression and hypocalcemic seizures in the newborn. Fewer than 20 similar cases have been reported in the past century of literature.
DISCUSSION
After ruling out multiple syndromes contributing to our patient's hyperparathyroidism, it was concluded that our patient suffered from isolated multiglandular primary hyperparathyroidism. Fortunately, the infant in our case was able to recover parathyroid function over the course of 9 months of calcium supplementation. Not all cases of intrauterine parathyroid suppression are able to recover and wean from supplemental calcium [7]. Undiagnosed maternal hyperparathyroidism can lead to disastrous complications for infants and therefore must be considered in both hypercalcemic pregnant patients and hypocalcemic neonates. After 24–48 h, a child presenting with symptomatic hypocalcemia can represent a potentially fatal condition indicating severely suppressed parathyroid function and an underlying maternal hyperparathyroidism. This potentially fatal presentation of the disease highlights the importance of diagnosis and treatment of hypercalcemia in the pregnant patient. We recommend considering surgery at the time of diagnosis, even during pregnancy, to minimize dangers to both mother and infant.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- parathyroid
- parathyroid hormones
- pregnancy
- ultrasonography
- hyperparathyroidism
- hypocalcemia
- seizures
- ionized calcium
- calcium
- bone neoplasms
- cysts
- emergency service, hospital
- infant
- newborn
- laboratory techniques and procedures
- mothers
- multiple endocrine neoplasia type 1
- office visits
- parathyroidectomy
- preoperative care
- jaw
- hyperparathyroidism, primary
- seizures, clonic
- adenomatosis
- convulsions in the newborn
- sestamibi scan
- intrauterine route of drug administration
- undiagnosed
- symptom onset



