-
PDF
- Split View
-
Views
-
Cite
Cite
Varun Kapur, Merab Krikhely, I. Michael Leitman, Operative management of splenic rupture and hepatic flexure injury during diagnostic colonoscopy in a patient with adenocarcinoma of the cecum, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv021, https://doi.org/10.1093/jscr/rjv021
Close - Share Icon Share
Abstract
Diagnostic colonoscopy has evolved to become the gold standard for the screening for carcinoma and other diseases of the colon. Injuries to the colon are rare and may be managed in a variety of ways. This includes observation and bowel rest or operative intervention and repair. Other organs are at risk during colonoscopy. The present report describes a patient who underwent colonoscopy for the work-up of anaemia. Following colonoscopy she developed signs of haemorrhagic shock and was found to have haemoperitoneum. She underwent surgery, and adenocarcinoma of the cecum was identified and managed during exploration. The clinical management is described.
INTRODUCTION
Perforation of the colon is a significant and well-recognized complication of fiberoptic colonoscopy. Splenic rupture is even less common and a potentially life-threatening complication of colonoscopy. Presentation can be delayed for hours or days after discharge and therefore not easily diagnosed without imaging. We report a case of diagnostic colonoscopy complicated by splenic injury and avulsion injury to right mesocolon in a patient, who was also found at surgery to have a cecal mass.
CASE REPORT
The patient was a 76-year-old female who presented for an outpatient upper gastrointestinal endoscopy (EGD) and a colonoscopy as a work-up for iron deficiency anaemia. She had a significant past medical history with coronary artery disease and previously underwent percutaneous coronary intervention with stents 4 years prior. She was on aspirin. There was no prior history of prior abdominal surgery. She underwent bowel preparation with a polyethylene glycol solution. She underwent EGD and colonoscopy under monitored sedation. Suring colonoscopy, the bowel preparation was noted to be adequate but the colonoscopy procedure was noted to be technically difficult with looping experienced especially in the transverse colon and hepatic flexure. External manual pressure was also applied. Repeated attempts to visualize beyond the hepatic flexure were unsuccessful, after which the procedure was aborted. No lesions or polyps were visualized. She tolerated the procedure well and reported no complaints immediately after. One hour after the endoscopy, the patient complained of light-headedness when trying to get out of bed, with an episode of syncope.
She complained of shortness of breath and chest pain. Vital signs were notable for pulse of 110/min, blood pressure 110/70 mmHg, respiratory rate of 20/min. On physical examination, she appeared uncomfortable, diaphoretic and pale. The abdominal exam was benign. Laboratory work-up was remarkable for haemoglobin of 8.5 mg/dl (preoperative hemoglobin was 9.5 mg/dl). Given her prior history of coronary artery disease, she underwent an electrocardiogram and serum troponin levels were normal. A portable upright chest X-ray was found to be negative for pneumoperitoneum, effusions or infiltrates (Fig. 1).

Upright portable chest X-ray without evidence of pneumoperitoneum, effusions or infiltrates.
She underwent immediate CT scan of the chest, abdomen, and pelvis with oral and intravenous contrast. During the preparation for the CT scan, she began to complain diffuse of abdominal pain. Her physical examination was now remarkable for a soft but diffusely tender abdomen. The pulse remained between 110 and 120/min and the blood pressure was 90/60. After 3 h, the hemoglobin was 6.1 mg/dl.
CT scan (Figs 2 and 3) revealed a large hematoma at the lateral margin of the spleen that displaced the spleen medially and compresses its lateral margin. A moderate amount of relatively low attenuation fluid also tracked into the right paracolic gutter and perihepatic space. There also appeared to be a 3.5 × 2.5 cm broad-based mass along the wall of the right colon. The CT scan of the chest also demonstrated a pulmonary embolus in a subsegmental artery of the right upper lobe. Given these findings, the patient was aggressively resuscitated with packed red blood cells and taken emergently to the operating theatre.
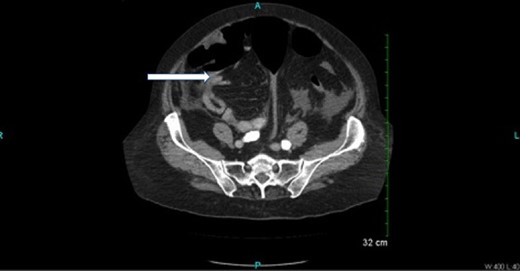
Oral and intravenous contrast enhanced CT of the abdomen demonstrating air within the colonic lumen and a 3.5 × 2.5 cm broad-based mass along the wall of the right colon (white arrow).
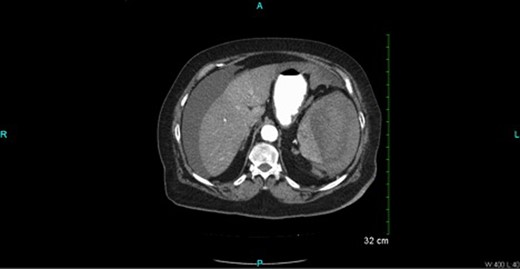
Oral and intravenous contrast-enhanced CT of the abdomen demonstrating air within the colonic lumen and a large haematoma at the lateral margin of the spleen that displaced the spleen medially, compressing its lateral margin. A moderate amount of relatively low attenuation fluid is also seen tracking into the right paracolic gutter and perihepatic space.
At surgery, an exploratory laparotomy was performed. About 1.5 l of fresh blood and 1 l of blood clots were encountered with active bleeding around a shattered spleen. Splenectomy was performed. Further exploration revealed a large hematoma around the hepatic flexure with avulsion of mesocolon causing visible evidence of ischaemia to the right colon. A mass was palpated at the cecum. A decision was made to perform a right haemicolectomy. Since the patient was haemodynamically unstable requiring massive blood transfusion, a primary anastomosis was avoided and an end ileostomy was performed with a mucus fistula.
Following this procedure, an inferior vena cava filter was placed using fluoroscopic assistance.
Histological examination of the colon was remarkable for a 3 cm low-grade mucinous adenocarcinoma of the cecum. Mesenteric lymph nodes were negative for metastases (T2N0M0). The patient made an uneventful recovery and was discharged home on the eighth postoperative day with plans to reverse the ileostomy in about 6 weeks.
DISCUSSION
The most common complication associated with colonoscopy is colonic perforation (0.1–2.67%) and haemorrhage (0.001–2.5%), as described in multiple reviews of post-colonoscopy complications [1]. Serious colonic injuries are more frequent during therapeutic. Small perforations mostly result from direct mechanical trauma, such as the result of forceful passage of the tip of the endoscope through a diverticulum, inadvertent penetration of the side of a tight flexure or bend, or tearing during traversal of a narrowed stricture [2]. The most common site of colonic injury is to the sigmoid colon followed by the cecum [3, 4]. Injury to the right colon, hepatic flexure occurs less frequently.
The true incidence of splenic rupture is unknown with around 100 published case reports [5]. The most likely mechanism for this complication is tension on the splenocolic ligament, or from pre-existing adhesions, or both, due to manipulations of the sigmoid, descending colon, or transverse colon, or resulting passage of the endoscope through the splenic flexure resulting in parenchymal tears or avulsion of the spleen [6, 7].
The use of aspirin and non-steroidal anti-inflammatory drugs has not been associated with an increased risk of bleeding after colonoscopy [8].
Splenic injuries after colonoscopy may be underreported and cases may remain undetected [1] and continue to remain a cause of concern. The diagnosis of splenic rupture may be delayed and could lead to a poor outcome. Although computerized tomography is highly sensitive, suspecting this complication is the best way to assist in the early diagnosis [1]. Patients with abdominal pain, hypotension and a drop in haemoglobin without rectal bleeding after colonoscopy should be suspected of having splenic injury [1].
The factors associated with splenic injury include difficulty intubating, looping of the instrument, traction on the splenocolic ligament, adhesions between the colon and spleen and the presence of a large polyp or mass at the splenic flexure [9]. Excessive external pressure on the left hypochondrium to facilitate scope passage can simulate blunt trauma [9]. Other risk factors include female gender and advanced age [10].
CONFLICT OF INTEREST STATEMENT
None declared.



