-
PDF
- Split View
-
Views
-
Cite
Cite
Kevin Behm, David W. Larson, Dorin Colibaseanu, Intravenous immunoglobulin use in managing severe, perioperative peristomal pyoderma gangrenosum following subtotal colectomy with end ileostomy for medically refractory chronic ulcerative colitis, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv019, https://doi.org/10.1093/jscr/rjv019
Close - Share Icon Share
Abstract
Peristomal pyoderma gangrenosum (PPG) is a rare subtype of pyoderma gangrenosum that is characterized by painful, necrotic ulcerations occurring in the area surrounding an abdominal stoma. PPG is typically seen in younger patients with active inflammatory bowel disease. The etiology and pathogenesis is largely unknown and risk factors are not well defined. Therapy typically involves a combination of aggressive local wound care and systemic medications. Diagnosis and management of PPG can be difficult and data on treatment are limited. We present a case of severe postoperative peristomal recalcitrant to conventional therapy successfully treated with intravenous immune globulin.
INTRODUCTION
Peristomal pyoderma gangrenosum (PPG) is a rare subtype of pyoderma gangrenosum (PG) that is often challenging to diagnose and manage effectively. Treatment algorithms are not well defined and PPG is frequently refractory to conventional therapies. We present a case of severe recalcitrant PPG in the immediate postoperative period effectively treated with a multidisciplinary, multimodality approach including aggressive local wound care, antibiotics, mycophenolic acid, prednisone and intravenous immunoglobulin.
CASE REPORT
A 56-year-old male with a history of chronic ulcerative colitis (CUC) was admitted to the hospital for an acute CUC exacerbation. The patient was placed on bowel rest and high-dose steroids. Biologic agents were deemed too high risk given the patient's history of papillary thyroid cancer and cutaneous melanoma. His symptoms failed to improve, so he underwent a laparoscopic subtotal colectomy with an end ileostomy for medically refractory CUC. The patient's postoperative course was uncomplicated and he was discharged on postoperative day (POD) 2.
On POD 7, he presented with stomal separation and mild cellulitis. He was treated with local wound care and oral antibiotics. Patient was re-evaluated on POD 14 for worsening pain and erythema. His antibiotic regimen was changed with temporary improvement in both pain and erythema; however, on POD 20 the patient presented with worsening pain, erythema and formation of a parastomal ulcer (Fig. 1). The patient was admitted to the hospital for aggressive wound care and intravenous antibiotics. The progression of the ulceration and the jagged undermined border of the ulcer with associated pustulation were suspicious for acute presentation of PPG. Pathologic examination of the wound punch biopsy verified this based on the histologic presence of acute neutrophil infiltration. After multidisciplinary discussion between surgeons, gastroenterologists, infectious disease and dermatology, therapy was expanded to ertapenem, vancomycin, prednisone 60 mg daily and intravenous immune globulin (IVIG) 2 g/kg in divided doses over 3 days. IVIG was chosen as adjunct therapy due to the severity of the disease and the patient's history of previous malignancies. In addition, local wound care was continued with tacrolimus ointment and silver sulfadiazine cream twice daily. Over the next 4 days, his wound showed dramatic improvement (Fig. 2). On POD 27, the patient was discharged to complete a 14-day course of ertapenem and vancomycin, a prolonged course of 60 mg of oral prednisone daily and IVIG every 4 weeks given as 2 g/kg in divided doses over 3 days.
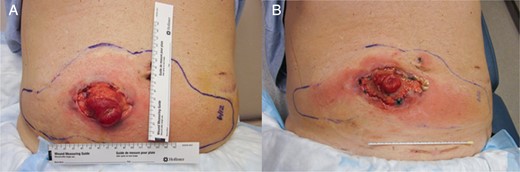
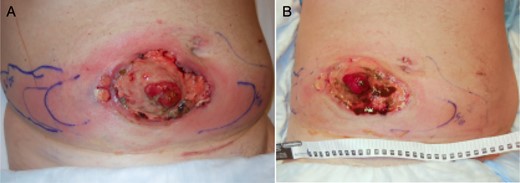
Improvement with multimodality treatment, from Day 23 (A) to Day 26 (B).
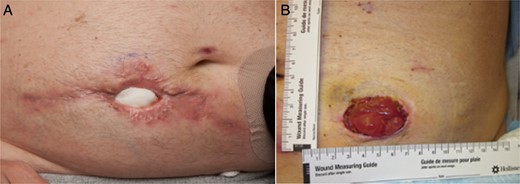
On POD 34, the patient was taken to the operating room with acute presentation of a mechanical bowel obstruction due to a parastomal hernia and underwent repair of parastomal hernia and stoma resiting. The patient's hospital course was uncomplicated and he was subsequently discharged after 3 days. Patient evaluation 40 days from his original operation revealed no signs of PPG at his new stoma site, but active PPG in his previous ileostomy site. The patient was started on mycophenolic acid 500 mg twice daily in addition to his current therapy of prednisone 60 mg daily and IVIG every 4 weeks given as 2 g/kg in divided doses over 3 days due to the presence of active disease. Outpatient evaluation on POD 70 (Fig. 3) showed a dramatic improvement in his wound with no active disease and he was started on a prednisone taper with the goal to discontinue his immunomodulator therapy in a stepwise fashion. There have been no signs of recurrence 9 months following successful treatment, and current therapy consists of prednisone 10 mg daily and mycophenolic acid.
DISCUSSION
PPG is a rare subtype of PG that is typically seen in patients with active inflammatory bowel disease (IBD) [1]. Diagnosis and management of both PG and PPG can be difficult. Goals of therapy are to control inflammation, reduce pain, optimize wound healing and minimize exacerbating factors [2]. Standard first-line therapy for PG is based on disease severity at the time of presentation. Mild local disease is typically managed with high potency topical corticosteroids, topical tacrolimus and oral antineutrophil agents in combination with local wound care to keep a moist environment while limiting unnecessary trauma [2]. For large or rapidly progressing lesions, first-line systemic therapy includes corticosteroids, cyclosporine and infliximab in patients with Crohn's disease. In cases where first-line therapies fail, an array of other immunomodulatory agents can be utilized as adjuncts. For severe refractory cases, IVIG or alkylating agents may be utilized in combination or as monotherapy. PPG is typically managed using the same algorithms outlined to treat PG, despite the increased prevalence of refractory cases. Funayama et al. [3] reported that early detection and treatment of PPG with moderate- to high-dose corticosteroids can be effective for promoting early wound healing. In a large case series, Sheldon et al. [4] concluded that surgical resection of all active IBD in combination with medical therapy is usually required for patients with active IBD. It is important to note that direct approaches for stoma relocation, ulcer excision or skin grafting have poor results and are not recommended [5]. Quality data on treatments for both diseases are limited, and further studies are required to determine the best treatment algorithm.
To our knowledge, this is the first study describing IVIG as an adjunct therapy for successful treatment of severe postoperative PPG and only the second report of PPG in the immediate postoperative period. This case report describes a multidisciplinary, multimodality approach to the treatment of a patient with PPG recalcitrant to conventional treatment, who was treated successfully with aggressive local wound care, antibiotics, mycophenolic acid, prednisone and IVIG.
ACKNOWLEDGEMENTS
The authors acknowledge Academic and Research Support at Mayo Clinic in Florida for their assistance.
CONFLICT OF INTEREST STATEMENT
None declared.



