-
PDF
- Split View
-
Views
-
Cite
Cite
Luciano Zogbi, Camila Juliano, Aluísio Neutzling, Atypical fibroxanthoma, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv010, https://doi.org/10.1093/jscr/rjv010
Close - Share Icon Share
Abstract
Atypical fibroxanthoma (AFX) is a rare skin neoplasm of low-grade malignancy and fibroblastic origin. AFX is a curable cutaneous disease and the diagnosis depends on knowledge of its clinical and histological features and combined immunohistochemistry markers. This study presents a case of a male patient, aged 90 years, presented with painless skin lesion in his ear. The lesion had been growing progressively for 2 months, measured ∼1.5 cm, ulcerated, fixed and firm. After a biopsy, the patient underwent a complete resection with adequate surgical margins and showed favorable evolution without complications or recurrence. The histopathological evaluation showed a poorly circumscribed ulcerated dermal nodule, mesenchymal proliferation, with pleomorphic spindle cells. There was infiltration of the deep dermis and subcutis, showing malignant features, but there was no invasion of cartilage. The immunohistochemical analysis confirmed the diagnosis of AFX.
INTRODUCTION
Atypical fibroxanthoma (AFX) is a rare neoplastic skin disease, responsible for ∼0.2% of malignant skin cancers. AFX was first reported by Helwig in the early 1960s and is characterized as a neoplasm of low-grade malignancy of fibroblastic origin. AFX generally occurs on the actinic-damaged skin of the elderly, especially on the face and scalp. AFX can exhibit various growth patterns and often presents as an elevated, well-delineated nodule limited to the dermis, partially extending into the subcutaneous fatty tissue. The epidermis is atrophic and can be ulcerated. The tumor comprises atypical spindle and epithelioid cells with pleomorphic vesicular or hyperchromatic nuclei. Often atypical multinucleated giant cells, mitoses and numerous blood vessels are observed. Despite these clinical and histopathological features, the diagnosis of AFX should be confirmed by immunohistochemistry (IHC), to exclude the possibility of other diseases such as carcinoma, melanoma and malignant fibrous histiocytoma (MFH) [1–5]. The aims of this study are to report a case of this disease and present a brief and updated literature review.
CASE REPORT
A white male, 90 years old, complained of a painless skin tumor in the right ear, a progressive growth, 2 months ago. The tumor presented as a nodular lesion, ulcerated, firm and measuring ∼1.5 cm, as seen in Fig. 1. One year ago, he had a basal cell carcinoma on his leg that presented no complications or recurrence. After an incisional biopsy of the tumor in his ear, the patient underwent a complete resection with free margins, including cartilage, under local anesthesia (Figs 2 and 3).

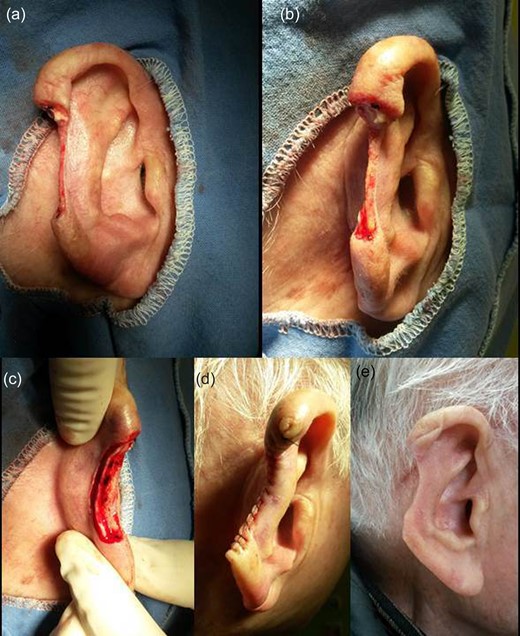
Tumor removal. (a) Anterior view, (b) lateral view, (c) posterior view, (d) immediately postoperative and (e) 60th postoperative day.
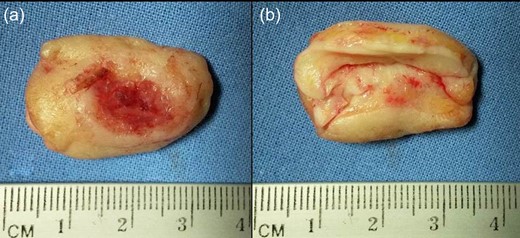
Surgical specimen. (a) Anterior view and (b) posterior view. Special detail of cartilage removed en bloc with free margins.
Macroscopic pathologic examination revealed a skin sample measuring 3.2 × 2.5 cm, showing epidermis with a nodular, ulcerated and hyperchromic lesion measuring 1.3 × 0.2 cm. Histologically, there was a poorly circumscribed dermal nodule, ulcerated, comprising mesenchymal proliferation with pleomorphic spindle cells arranged in a disorderly, fascicular and storiform pattern. The nodule was infiltrative in the deep dermis and subcutis (Fig. 4a), showing some malignant features, such as bizarre nuclei, exuberant nucleoli and a few atypical mitotic figures. Some multinucleated giant cells and dilated capillaries were also observed within the tumor (Fig. 4b). A mononuclear inflammatory infiltrate was also associated. Vascular and perineural invasion were not identified nor was there invasion of cartilage (Fig. 4c). The tumor had surrounded but not destroyed adnexal structures.
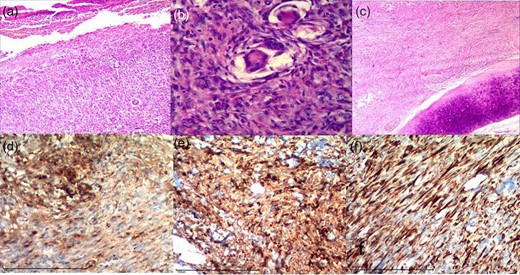
Above: photomicrographs of sections stained with hematoxylin–eosin: (a) presence of ulceration (×100), (b) presence of nuclear atypia, mitoses and giant cells (×400) and (c) presence of deep dermis and subcutis invasion; free cartilage (×100). Below: photomicrographs of IHC analysis with the following markers: (d) alpha-1-antitrypsin, (e) CD68 and (f) vimentin.
IHC analysis was used to search for specific antigens using the Automated Ventana BenchMarkR XT System. The main findings of the IHQ analysis are described below (Figs. 4d–f): The above data confirmed the diagnosis of AFX. The patient had a favorable postoperative course without complications or recurrence at a 1-year follow-up (Fig. 2e).
Positive markers: alpha-1-antitrypsin (polyclonal; Fig. 4d), CD68 (clone KP1; Fig. 4e), vimentin (clone V9; Fig. 4f) and KI-67 (clone SP6).
Negative markers: cytokeratin (clones AE1 and AE3), CD34 (clone QBEnd 10), PS100 (anti-human S-100) and epithelial membrane antigen (EMA) (clone E29).
DISCUSSION
The clinical features of this case, although nonspecific, were the most typical described in the literature: a solitary skin tumor growing for several months, nearly exclusively on the sun-damaged skin of the elderly, mainly on the head and scalp, but especially on the ears. AFX affects two-thirds of more Caucasian males than males of other races. On physical examination, the most common form of AFX is a painless, firm, solid, immovable nodule, skin colored or brown-red and frequently ulcerated, exactly as our patient presented [1–5].
Histologically, these tumors resemble pleomorphic forms of MFH, commonly regarded as a variant, presenting a more superficial location. Size and depth are important in differentiating between AFX and MFH, which is generally larger and deeper. On histological analysis, AFX is a well-defined mesenchymal neoplasm characterized by the dermal proliferation of atypical spindled cells in a haphazard and disorderly pattern, with a variant degree of atypia. Cells with round and elongated nuclei with large cytoplasm and abundant eosinophilic nucleoli, forming bundles and fascicles oriented in various directions, can be observed. The most common morphological pattern is dominated by a mixture of spindle cells and epithelioid cells, followed by variants with predominantly spindle cells, exclusively spindle cells or predominantly epithelioid cells. This particular case had a predominance of spindle cells, ∼80%. A similar diversity exists for the tumor stroma, generally a collagenous, elastotic stroma predominates, which is what occurred in this patient and is commonly observed in fusiform mesenchymal neoplasms. Pleomorphic epithelioid cells also can be observed with occasional inflammatory cells. A storiform pattern is rarely evident, as presented in this case. The cells can exhibit multinucleation, pleomorphism, atypical mitosis and occasionally foam cells and macrophages. A differential diagnosis consists of distinguishing AFX from melanoma, spindled carcinoma, MFH, dermatofibrosarcoma and others spindle-cell neoplasms in which IHC analysis is fundamental. Absent immunostaining for cytokeratins, S100 and HMB45 are helpful in excluding both carcinoma and melanoma. A histiocytic/macrophage marker (CD68) is positive in more than half of all AFX cases [1, 4–6]. The initial diagnosis was malignant mesenchymal neoplasm suggestive of low level sarcoma, requiring IHC analysis. This neoplasm was positive for CD68, vimentin, Ki-67 and alpha-1-antitrypsin as well as negative for cytokeratins, S100, CD34 and EMA, confirming the diagnosis of AFH.
Surgery is the therapy of choice, and a wide excision with safety margins >1 cm should be the goal. We performed a wide excision on this patient, taking off part of his ear to remove >1 cm of margin and offer him the greatest chance of a cure. After complete excision, a cure may be presumed: recurrences generally appear from several months to 2 years after the primary excision. After 1 year of follow-up, this patient maintained good condition, showing no recurrence. Metastasis occurs primarily in incompletely excised tumors, as well as in tumors with involvement of the subcutis or deeper structures, tumor necrosis or perineural or vascular invasion [1, 6–8]. Although microscopic analysis showed that the tumor was infiltrative deep into the dermis and subcutis with malignant features, vascular and perineural invasion were not identified, nor was an invasion of the cartilage and the tumor had wide-free surgical edges.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
We thank Drs Ana Geyger and Luis Fernando Rivero, from the Laboratório Patologistas Reunidos/POA for IHC analysis.
REFERENCES
Author notes
This study was performed with the patient's written informed consent.



