-
PDF
- Split View
-
Views
-
Cite
Cite
Avtar Sur, Hartej Sur, Muhammed A. Khan, Laparoscopic-assisted endoscopic retrograde cholangiopancreatography post bariatric surgery: how to overcome the technical challenges, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv011, https://doi.org/10.1093/jscr/rjv011
Close - Share Icon Share
Abstract
The prevalence of bariatric surgery is increasing worldwide and as a direct consequence, there shall be an increasing number of patients presenting with the complications of bariatric surgery, often to non-specialist units. The authors report a case of a 42-year-old Caucasian female who had previous laparoscopic Roux-en-Y gastric bypass, open cholecystectomy and abdominoplasty presenting with right upper quadrant pain in keeping with retained common bile duct stones. After the failure of conservative management, a laparoscopic-assisted transgastric endoscopic retrograde changiopancreatography and sphincterotomy was performed. We shall be describing our technique.
INTRODUCTION
The World Health Organization estimates that there are 500 million obese individuals worldwide. Currently for super-obese individuals, bariatric surgery is the only evidence-based approach that results in clinically significant and sustainable weight loss [1].
With the increasing prevalence of obesity, there is an increased demand for bariatric surgery. Subsequently, a large number of patients shall be presenting with the complications of bariatric surgery [2]. We present a case that highlights one such complication and its novel management.
CASE REPORT
A 42-year-old Caucasian female underwent laparoscopic Roux-en-Y gastric bypass in February 2007. She subsequently developed gallstones, a known complication of bariatric surgery due to rapid weight loss. This was managed by an open cholecystectomy in November 2007. An abdominoplasty was performed in 2010 to remove excess skin.
She presented to our unit in February 2012 with a week long history of right upper quadrant pain associated with vomiting. Blood tests revealed deranged liver function tests: alkaline phosphatase of 169 U/l and alanine aminotransaminase of 188 U/l. Interestingly, her Bilirubin was <5 U/l. Ultrasound revealed a mildly dilated common bile duct of 9.5 mm. A computed tomographic scan was organized confirming the appearances of a dilated common bile duct and the potential of a calcified stone in the common bile duct.
She was managed conservatively with analgesia and ursodeoxycholic acid to attempt to dissolve the stones. Her liver function tests and pain improved, and she was discharged with an outpatient magnetic resonance cholangiopancreatography (MRCP).
In March 2012, her MRCP showed a dilated common bile duct of 10 mm and two small filling defects suggestive of gallstones. She represented to hospital in April 2012 with similar symptoms. On this occasion, a percutaneous transhepatic cholangiogram was arranged. Again, this confirmed the dilated common bile duct, but also showed free drainage of bile into the duodenum and no gallstones; hence, therapeutic interventions were not undertaken.
She was referred to the gastroenterologists for further advice, but as of June 2012 she was still symptomatic.
Ultimately, an endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy was deemed to be necessary to alleviate her symptoms.
Owing to the altered anatomy post Roux-en-Y gastric bypass, this was to be a technical challenge. Post procedure, the patient is left with a small gastric pouch. The bypass of the distal stomach and proximal small bowel is achieved by anastomosis of the gastric pouch and the jejunum known as the Roux alimentary limb. The biliary pancreatic limb is then anastomosed to a small bowel [3]. As a result it is technically challenging to perform an ERCP in the conventional manner, success rates have been quoted as well below 70% [4].
What was performed was a laparoscopic-assisted transgastric ERCP and sphincterotomy. We shall describe our technique as follows.
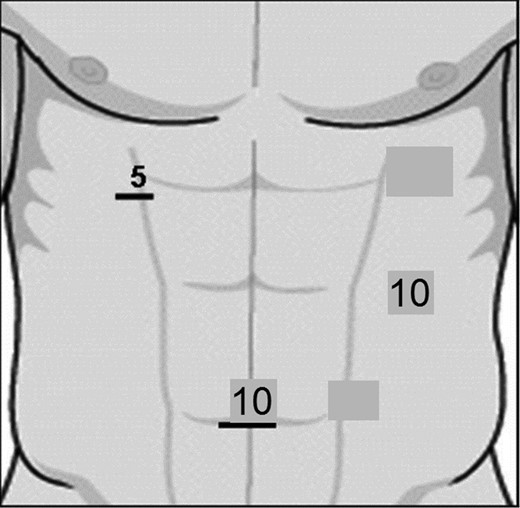
The patient was positioned in the classic Lloyd Davies position. She was prepped and draped in the conventional manner. Carbon dioxide pneumoperitoneum was achieved through the standard 10-mm umbilical port. This was technically challenging in our patient due to the altered anatomy post abdominoplasty. Two subsequent port sites were used: a 5-mm port site in the right upper quadrant and a 10-mm port in the left hypochondrium (Fig. 1).
The port site in the left hypochondrium allows the gastric remnant to be visualized. A site on the greater curvature of the stomach was chosen. A gastrotomy was performed using diathermy. Stay sutures were placed in a diamond-shaped configuration around the gastrotomy site—these can allow both traction and counter-traction.
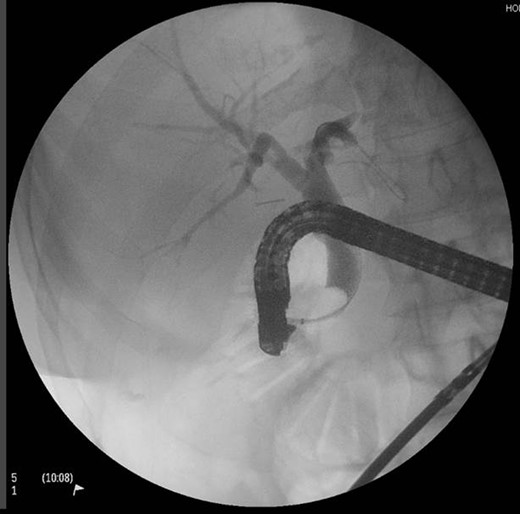
A sterile ERCP scope inserted manually through a left 10-mm port site all under laparoscopic visualization. ERCP and sphincterotomy were performed in the conventional manner by the consultant gastroenterologist. There were no obvious gallstones in our patient (Fig. 2).
The gastrotomy site was closed with a two layer closure: the first layer as a running stitch and then as a horizontal mattress with 2.0 vicryl. The procedure was uneventful. She was admitted for an overnight stay and discharged the following day. Upon review of the patient in a routine 6-week follow-up clinic, she was asymptomatic and was discharged back to the care of her general practitioner.
DISCUSSION
With the increased demand for bariatric surgery worldwide, there will be an increased role of endoscopy to diagnose and manage complications.
With altered anatomy, the transgastric approach can be used as an access point into the gastrointestinal tract. We have demonstrated that the technique when performed correctly can be a safe and viable option in most district general hospitals, which would certainly have a laparoscopic surgeon and a gastroenterologist on site.
CONFLICT OF INTEREST STATEMENT
None declared.



