-
PDF
- Split View
-
Views
-
Cite
Cite
Michael Knoop, Manon Weinhold, Andreas Becker, Missing pancreatic isthmus during pancreaticoduodenectomy, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv009, https://doi.org/10.1093/jscr/rjv009
Close - Share Icon Share
Abstract
Pancreatic malformations usually represent a surgical challenge, however, depending on the anatomical location even complex procedures such as pancreatic head resection may be facilitated. In a 78-year-old-woman the unique observation of a missing pancreatic isthmus was made during pylorus-preserving pancreaticoduodenectomy for pancreatic ductal adenocarcinoma. Resection of the pancreatic head could be performed without the usual cross-section at the isthmus, the pancreatic remnant was drained by pancreaticogastrostomy. Complete agenesis of the dorsal pancreas with missing neck, body and tail of the pancreas has been shown to be associated with malignant pancreatic tumors, as demonstrated in this case of partial agenesis (missing isthmus) of the dorsal pancreas. The missing pancreatic isthmus is a unique, not yet described finding during pancreatic exploration for tumor resection. In the absence of previous abdominal trauma, a partial agenesis of the dorsal pancreas could explain this malformation.
INTRODUCTION
The complex embryologic morphogenesis of the pancreatic gland by fusion of the dorsal and ventral bud of the primordial foregut possibly results in congenital anomalies that remain asymptomatic and are found incidentally during clinical imaging [1]. Other variants of pancreas and pancreatic ducts may cause recurrent pancreatitis or gastric outlet obstruction, could require surgical correction or become important for planning of pancreatic procedures [2] .We describe the unique incidental finding of a missing pancreatic isthmus in a patient undergoing pancreaticoduodenectomy for periampullary cancer.
CASE REPORT
A 78-year-old woman with metabolic syndrome and chronic obstructive pulmonary disease developed obstructive jaundice and underwent endoscopic biliary stenting and papillotomy for suspected periampullar carcinoma (double-pigtail endoprothesis, 10 Fr./7 cm). Histology revealed a moderately differentiated bile duct carcinoma. Cytopathology showed a class V PAP stain with adenocarcinoma cells. The abdominal computed tomography displayed an inhomogenous hypodense tumor in the pancreatic head of 2 cm diameter with no signs of metastatic spread. The proximal part of the pancreatic corpus seemed to be atrophic (see Fig. 1). Endosonography demonstrated a tumor of the ampulla of Vater with a size of 20 × 23 mm and infiltration of the duodenal wall (at least uT2uN1).
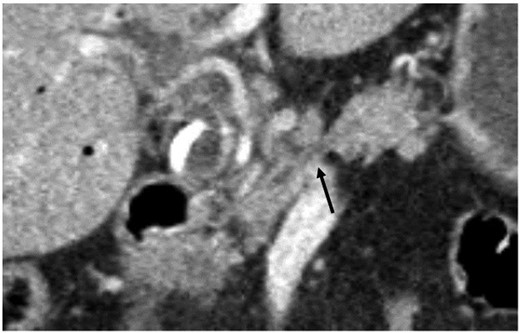
Coronary abdominal CT scan: missing pancreatic isthmus with isolated pancreatic duct (arrow).
Three weeks after biliary stenting the patient underwent pylorus-preserving pancreaticoduodenectomy according to Longmire-Traverso with insertion of the pancreatic remnant in the posterior gastric wall (pancreaticogastrostomy). During dissection we encountered a missing pancreatic isthmus between the pancreatic head and the body with a completely free duct of Wirsung crossing ventrally the portal vein (see Fig. 2). The end of the pancreatic body was cone shaped with the emerging duct at its tip. The duct was transsected and stented for later anastomosis. Owing to this anomaly the pancreatic head could be removed without any transsection of pancreatic parenchyma. There were no other obvious anatomical variations in the upper abdomen.
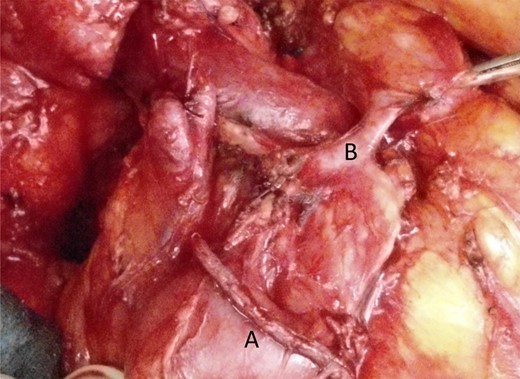
Situs after pylorus-preserving transsection of the duodenum with stapled duodenum (A) and pancreatic duct (B) crossing the portal vein.
Histology showed a ductal pancreatic carcinoma with invasion of the ampulla of Vater (pT3pN1(1/4) pL1 pV0 Pn1) with tumor-free resection margins (R0).
The postoperative course was uneventful and the patient was released from hospital on POD 15.
DISCUSSION
The ventral bud of the duodenum gives rise to the lower head and uncinate process of the pancreas, the dorsal bud develops into the upper head, isthmus, body and tail of the pancreas [3]. Developmental failure of the dorsal bud results in partial or complete agenesis of the dorsal pancreas including neck, body and tail. This extremely rare condition seems to be associated with diseases such as hyperglycemia, diabetes mellitus, pancreatitis and abdominal pain [4] but may correlate with a higher incidence of pancreatic tumors as well [3, 5]. The missing pancreatic isthmus found in this case possibly represents a partial agenesis of the dorsal pancreas and fits to the observation of concurrent pancreatic ductal adenocarcinoma [5].
The pancreatic isthmus is an important surgical landmark. The isthmus represents the usual cross-section site of various oncologic pancreatic resections like pancreatic head or subtotal left pancreas resection [6]. The isthmus and the adjacent proximal body of the pancreas are the common site of pancreatoenteric anastomosis either as pancreaticojejunostomy or as pancreaticogastrostomy in various techniques [7].
The pancreatic isthmus links with a thin layer of parenchyma head and body of the pancreas, however, unusual contours or areas of fatty replacement can mimick a neoplasm [8]. In the preoperative computed tomography an atrophic or missing proximal part of the pancreatic body was suspected and identified as a missing neck during surgery.
The isthmus is a typical site of parenchymal laceration or pancreatic duct injury after blunt abdominal trauma [9]. A limited traumatic laceration of the isthmus sparing the duct of Wirsung and leading to partial recovery could be a theoretical explanation, however, our patient had never an abdominal trauma.
An isolated agenesis of the pancreatic isthmus with an unaffected duct of Wirsung, as in our case, is a unique finding. This case demonstrates that pancreatic malformations can be associated with pancreatic neoplasms.



