-
PDF
- Split View
-
Views
-
Cite
Cite
Vishnu R. Mani, Leaque Ahmed, Minimally invasive surgical technique integrating multiple procedures with large specimen extraction via inguinal hernia orifice, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv158, https://doi.org/10.1093/jscr/rjv158
Close - Share Icon Share
Abstract
While laparoscopic surgery can be performed using small skin incisions, any resected specimen must still be able to fit through these opening. For procedures, such as cholecystectomies and appendectomies, this is not usually a problem; however, for large specimens such as bowel or large tumors, this becomes problematic. Currently, the standard technique is to attempt piecemeal removal of the specimen or enlarge one of the laparoscopic incisions, effectively creating a mini laparotomy. Creating a larger incision adds many of the drawbacks of open laparotomy and should be avoided whenever possible. In this article, we present a new technique of combining the repair of an inguinal hernia, umbilical hernia with a duodenal tumor resection in order to extract the specimen through the inguinal hernia orifice.
INTRODUCTION
Common procedures such as cholecystectomy, appendectomy and bowel resection can be done with minimally invasive techniques (MIT), which reduce surgical incision site complications and postop discomfort while also improving cosmetic outcomes [1]. Common to MIS is specimen retrieval via the port and often large specimens require mini laparotomy and doing so takes away many of the advantages of MIS over open surgery, to overcome this natural orifice specimen extraction (NOSE) has been proposed in certain cases where the specimen is extracted via transcolonic or transvaginal route [2]. Unfortunately, NOSE require specific conditions in order to be feasible.
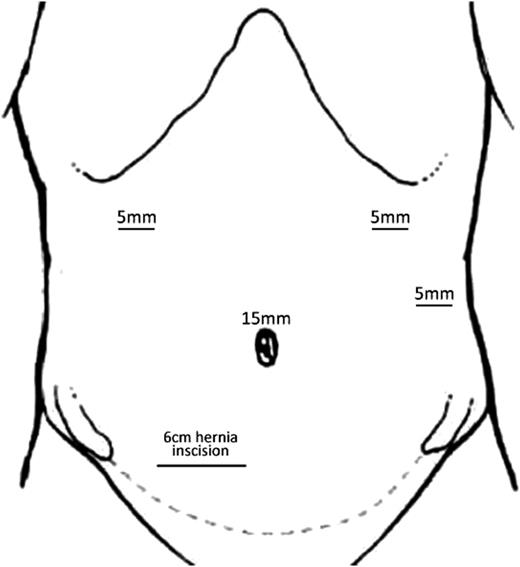
In this article, we present an alternative approach for specimen extraction. In an effort to maximize MIT, multiple operative procedures were combined to leverage the benefits of open and laparoscopic technique while reducing the total number of operative procedures. With over one million abdominal wall hernia repairs being performed every year in the USA [3], the prevalence of hernia is large enough that many patients will present with multiple surgical problems within a short period of time. These patients may be candidates for integrated surgical approaches, which can take advantage of multiple surgical techniques. In this article, we present an integrated approach for inguinal hernia and umbilical hernia repair with duodenal neuroendocrine tumor resection and small bowel anastomosis (Figure 1).

CASE REPORT
A 62-year-old male with bloody diarrhea was referred to surgery for management of duodenal mass. Evaluation by EGD, computed tomography (CT) imaging and elevated chromogranin indicated a possible neuroendocrine tumor. Further exam revealed umbilical and large right-sided inguinal hernia.
The patient was taken for elective laparoscopic possible open surgery, and pneumoperitoneum was created using a Veress needle. Three 5 mm trocars were placed: one on the midclavicular line below the right and one below the left costal margin, third in the anterior axillary line at the left costal margin, and a 15 mm trocar was placed in the midline, through the large umbilical hernia defect. Intraoperative endoscopy-assisted resection of the tumor was done extending from the gastric incisura to beyond duodenal bulb with clear margins and placed in the endopouch and moved intracorporeally toward the planned hernia incision site and left in situ, then antecolic antegastric Gastrojejunostomy was performed and Petersen's defect closed.
A 6 cm incision 2 cm superior to the right pubic tubercle was made, large indirect sac was found, dissected free of the cord and suture ligated. Lichtenstein procedure was performed for the repair of the defect. At this time, the tumor specimen placed in the endopouch was removed via hernia orifice.
Finally, the umbilical trocar was removed, and the umbilical hernia defect was repaired. Total surgical time was 105 min, blood loss estimated at <25 ml. Postoperative period was uneventful. Patient was discharged after 3 days with no complications. Pathological finding confirmed Grade I well-differentiated neuroendocrine tumor involving the mucosa and submucosa of the duodenum with foveolar metaplasia. After 2 years of regular follow-up with surgery, hematology and oncology, CT and octreotide scan for neuroendocrine activity, there has been no sign of further recurrence of the tumor.
DISCUSSION
One of the primary advantages of laparoscopic surgery over open laparotomy is the reduced sequelae of having a large incision site that predisposes to potential surgical site infection that accompanies varying grades of morbidity. Smaller surgical incisions tend to have less postoperative discomfort and hospital days, minimal surgical site infection, faster return to daily activities and superior long-term cosmetic results with overall reduced financial burden and better efficacy (Figure 2) [4]. Extending a laparoscopic port incision to accommodate extraction of a large specimen depletes many of the advantages of the laparoscopic surgery. In some cases, it may be possible to dissect the specimen and remove it piecemeal; however, in many cases involving malignancies, this is undesirable and may cause seeding of cancer cells. Combining multiple surgeries together allows the surgeon to combine common steps between the various procedures. For example, anesthesia only needs to be given once, fewer incisions are needed and only a single hospital visit is required for the patient. This greatly reduces the cost of the procedure for both the patient and the hospital.
In general, the risk of surgical site infection with bowel surgery is greater than without. Therefore, there may be increased risk of infection at the hernia repair site in this procedure [5]. However, with sparse data available on the subject, there has yet to be any evidence that shows this is the case. As more of these combined procedures are performed, there will eventually be enough data for evidence-based practice (Figure 3).

This case presented a specific scenario in which a patient with an umbilical hernia, right inguinal hernia and a duodenal tumor presented for surgery. In this case, removal of the tumor was immediately necessary, while the other two procedures could have been delayed for another time. In an effort to spare this patient from the risks of multiple procedures, it was decided that combining the procedures may result in a better outcome for the patient. The duodenal tumor was removed using standard laparoscopic technique; however, the specimen was removed through the opening created for the open right inguinal hernia repair.
The usefulness of such combination procedures will vary greatly from patient to patient. We hope that as such procedures are reported more often they will inspire other surgeons to attempt more creative combinations when opportunity presents, maximizing the advantages of minimally invasive methodology.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
There was no external funding in the preparation of this manuscript. We thank Apakama CP, MD and Lakshman Pradhan for their support in literature search in the preparation of the manuscript.



