-
PDF
- Split View
-
Views
-
Cite
Cite
Katsunori Asai, Shoichi Tani, Yukihiro Imai, Yohei Mineharu, Nobuyuki Sakai, Traumatic arteriovenous fistula of the superficial temporal artery, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv156, https://doi.org/10.1093/jscr/rjv156
Close - Share Icon Share
Abstract
Traumatic arteriovenous fistula (AVF) of the superficial temporal artery (STA) is rare. We report a case of surgically treated, histopathologically confirmed traumatic AVF of the STA. A 24-year-old male was admitted to our hospital after a traffic accident. Computed tomography scan on admission showed an acute epidural hematoma on the right surface of frontal lobe, which was emergently treated by surgical evacuation. One month later, he was aware of pulsatile tinnitus around the left ear. Digital subtraction angiogram showed an AVF, mainly fed by the left STA. After total removal of the fistula, his tinnitus immediately disappeared. Histopathological examination demonstrated that the artery was connected to the vein through the thin-walled vessels lacking internal elastic lamina and muscularized media, suggesting that the connecting vessels were newly formed.
INTRODUCTION
Traumatic arteriovenous fistula (AVF) is a pathology characterized by arteriovenous shunting secondary to blunt or penetrating trauma of artery and vein running in parallel, but AVF of the superficial temporal artery (STA) is rare. In this article, we report a case of histopathologically confirmed AVF of STA, which was surgically treated 1 month after surgery for right acute epidural hematoma caused by a traffic accident.
CASE REPORT
A 24-year-old male was admitted to our hospital after a traffic accident. Computed tomography scan had shown an acute epidural hematoma on the right surface of frontal lobe, which was emergently treated by surgical evacuation. One month later, he began to complain of pulsatile tinnitus in the left ear. A head magnetic resonance angiogram showed an extremely dilated vein in the left temporal region (Fig. 1). An angiography revealed a direct shunt between the left parietal branch of the STA and the superficial temporal vein (STV) in the preauricular region as well as an aneurysm in the left frontal branch of the STA (Fig. 2). He underwent surgery to remove the AVF and the aneurysm (Fig. 3). Pulsatile tinnitus disappeared immediately after surgery. Histopathological examination demonstrated that the artery was connected to the vein through the thin-walled vessels lacking internal elastic lamina and muscularized media, suggesting that the connecting vessels were newly formed (Fig. 4).
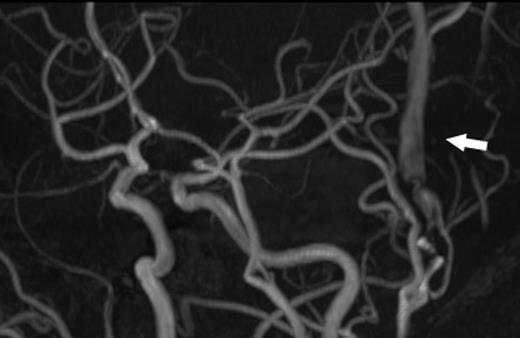
A magnetic resonance angiogram showed the dilated STV (arrow).
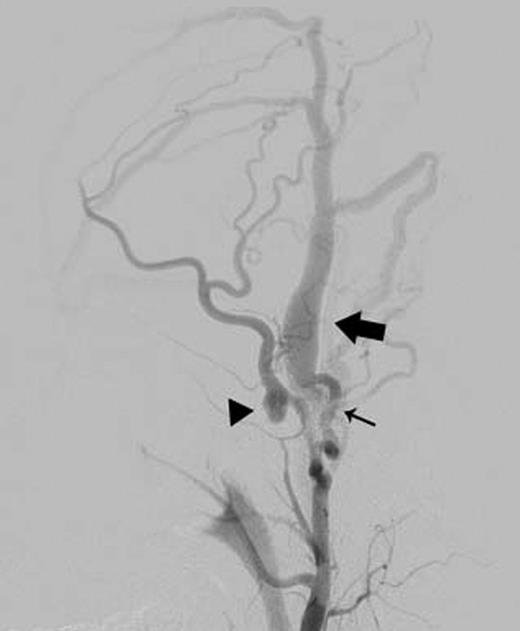
Left external carotid arteriography showed a high-flow AVF from the parietal branch of the STA (thin arrow) to the STV (wide arrow), and an aneurysm on the frontal branch of the STA (arrowhead).
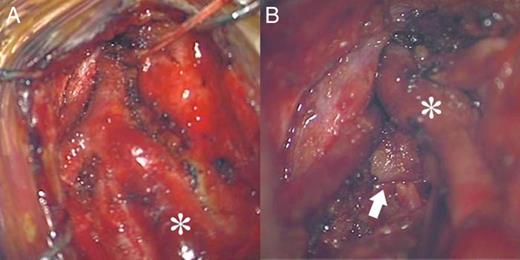
Intraoperative microscopic view. (A) The STV (asterisk) was extremely dilated and reddish. (B) The STA (arrow) was connected to the STV (asterisk).
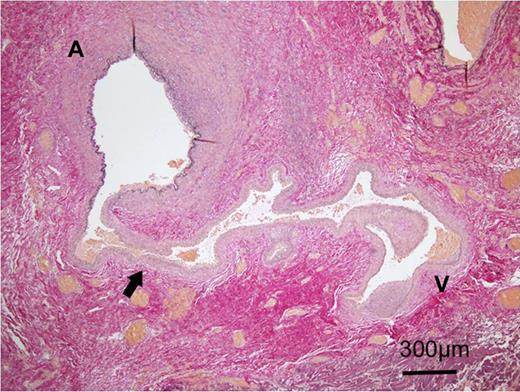
Histopathological photomicrograph with Elastica van Gieson stain showed that a thin-walled vessel lacking in internal elastic membrane (arrow) connected the artery (A) and the vein (V).
DISCUSSION
Blunt trauma to the STA may cause both aneurysm and AVF, but the incidence of AVF is lower than that of aneurysm, with a ratio of 23:131 [1], and only 36 cases have been reported as of 2007 [2]. As in this case, the preauricular region is one of the most commonly affected areas due to its anatomy: STA and STV run in parallel with each other over the temporal bone [2]. AVF lies around the ear cause pulsatile tinnitus [2, 3]. Traumatic AVF is treated with direct surgery or endovascular therapy. In direct surgery, since the block of the incoming blood vessel has a risk of recurrence [2], complete resection of the lesion is essential. Endovascular treatments include percutaneous coil embolization [4], embolization with liquid embolic agents such as isobutyl l-2-cyanoacrylate [5] or Onyx [3], direct-puncture coil embolization [6], and injection of absolute alcohol [7], all of which have been reported with good outcomes. However, AVF in the external carotid arterial system, which has potential complex collateral circulation, may be difficult to treat again if incomplete embolization ends in relapse [8]. Superficial focal fistula, like this case, can be cured by direct surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



