-
PDF
- Split View
-
Views
-
Cite
Cite
Benjamin L. Hodnett, Nicole C. Schmitt, Parthasarathy D. Thirumala, Umamaheswar Duvvuri, Intraoperative identification of the human communicating nerve during thyroidectomy, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv154, https://doi.org/10.1093/jscr/rjv154
Close - Share Icon Share
Abstract
The human communicating nerve (HCN) is a connection between the superior and recurrent laryngeal nerves that has been described in cadaveric studies. We report a case of an extralaryngeal variant of the HCN that was identified and stimulated intraoperatively during thyroidectomy. This appears to be the first case of intraoperative identification of this anatomic variant, of which the functional significance remains unclear.
INTRODUCTION
The basic description of laryngeal innervation involves the superior laryngeal nerve (SLN) providing ipsilateral sensory innervation to the supraglottis and motor innervation to the cricothyroid muscle, while the recurrent laryngeal nerve (RLN) provides sensory and motor innervation to all other laryngeal structures. However, anatomic studies suggest that there is significant overlap of motor and sensory innervation among branches of these nerves. Cadaveric studies of human larynges suggest a high prevalence of anastomoses between the internal and external branches of the SLN; between the internal branch of the SLN and the RLN, known in some instances as Galen's anastomosis; and finally, between the external branch of the SLN and the RLN, which has been termed the human communicating nerve (HCN) [1–3]. While cadaveric dissection studies have illustrated the complexity and prevalence of these nerve connections, their impact on laryngeal function is not well understood. Visualization of these nerve anastomoses in intact, non-dissected larynges is challenging. To our knowledge, intraoperative identification and electrostimulation of the HCN have not been previously described. We report a case where an extralaryngeal variant of the HCN was identified and stimulated during routine thyroidectomy.
CASE REPORT
The patient was a 56-year-old woman with an incidentally noted, 1.1 cm right thyroid nodule. The nodule had microcalcifications, and there was a suspicious central neck lymph node. Fine needle aspiration biopsy revealed papillary thyroid carcinoma. The patient elected to proceed with total thyroidectomy and central neck dissection. The Dragonfly neuromonitoring system was used. This system employs surface electrodes on the endotracheal tube that detect and record electromyographic activity from the thyroarytenoid muscles. In addition, stimulation-evoked muscle action potential was recorded including latency, amplitude and waveform morphology. During dissection of the right superior pole, the external branch of the superior laryngeal nerve (EBSLN) was identified. A nerve branch was noted originating from the EBSLN anterior to the cricothyroid muscle and coursing across the superior pole of the thyroid gland. This nerve then joined the main branch of the RLN prior to its laryngeal entry at the cricothyroid joint (Fig. 1) consistent with an extralaryngeal variant of the HCN. Stimulation of the EBSLN, but not the HCN, produced a strong twitch of the cricothyroid muscle. Stimulation of the HCN (set 100) at a current intensity of 0.5 mA produced a triggered compound muscle action potential with a peak latency and a peak-to-peak amplitude of 5.0 ms and 887.3 µV, respectively (Fig. 2A). Stimulation of the RLN at a current intensity of 0.5 mA produced a triggered compound muscle action potential with a peak latency and a peak-to-peak amplitude of 4.8 ms and 989.5 µV, respectively (Fig. 2B). Stimulation of the EBSLN at a current intensity of 0.4 mA produced a triggered compound muscle action potential with a peak latency and a peak-to-peak amplitude of 5.4 ms and 35.6 µV, respectively (Fig. 2C).
![Schematic of anatomic variant noted during thyroidectomy. The SLN terminated in its usual internal branch (IBSLN; sensory) and external branch (EBSLN) supplying motor fibers to the cricothyroid muscle. An extralaryngeal variant of the HCN was noted, connecting the EBSLN to the RLN prior to its laryngeal entry at the cricothyroid joint. Modified from Hodnett et al. [4].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2015/12/10.1093_jscr_rjv154/2/m_rjv15401.jpeg?Expires=1772272034&Signature=am~KvLelA7eOy8UbDywBtaduKwUSDbV8YDgfamnZEbpSZdU2XETpPDqUe4JTsWHOft2IMiA-18TWVmir77DSP~46vAejVt9~FUuEELcUp8YgJXhwN-N16nYozQpckgPTJr7b8Z60Yo5XwfpNZae9NhycUeyJXvicO1~SsHNE-03t6nPD2LlFhA5PanHzClrei8360mGwAIJs11MNmXgNZ6Fn~qDeqw3tZiBvz98z~~HGjy6w10NVH7gKzAWh~SXv07aVFX6FWhCi1Ids-CITLKU3rzvk8LsoPK3es5iT89gqHnwwux15GqrpGjeoiEwIzcwXHY-GEZisQDwdIBMrVw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Schematic of anatomic variant noted during thyroidectomy. The SLN terminated in its usual internal branch (IBSLN; sensory) and external branch (EBSLN) supplying motor fibers to the cricothyroid muscle. An extralaryngeal variant of the HCN was noted, connecting the EBSLN to the RLN prior to its laryngeal entry at the cricothyroid joint. Modified from Hodnett et al. [4].
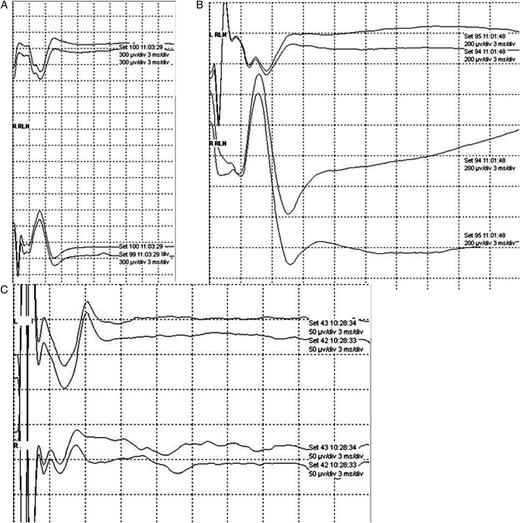
Stimulation of the HCN with the Dragonfly neuromonitoring system at 0.5 mA demonstrated a distinct waveform (A), with an onset latency of 3.2 ms and a peak-to-peak amplitude of 882.1 µV. This waveform was distinct from those produced by stimulation of the proximal RLN (B) or EBSLN (C). Note different scales used to best depict each of the responses.
DISCUSSION
Literature on the HCN consists primarily of cadaveric studies. The actual existence of the HCN was initially quite controversial, based on several cadaveric microdissection studies performed in the 18th, 19th and early 20th centuries showing mixed results [1]. A technique known as Sihler's stain, which clears soft tissue and counterstains nerves, has been useful for mapping fine nervous anastomoses in the human larynx that are difficult to discern with microdissection techniques [1, 2]. In a cadaveric study using Sihler's stain, Sanders et al. identified connections between the EBSLN and the RLN in 4 of 10 human larynges; the connection was intralaryngeal in all cases, with a branch of the EBSLN passing through the posterior surface of the cricothyroid muscle, then across the pyriform sinus before joining RLN branches in the thyroarytenoid muscle [2]. In a second study of 27 hemilarynges, the authors found EBSLN/RLN connections in 12 (44%) [1]. In one of these examples, the connection joined the EBSLN to the anterior branch of the RLN prior to its entry into the larynx and thyroarytenoid muscle, similar to the situation noted in our case. The finding of one extralaryngeal HCN among 27 hemilarynges suggests that the prevalence of this variant may be ∼3–4%. In a microdissection study of 90 human larynges, connections between the EBSLN and the RLN were noted in 68%, either at the point where the RLN innervated the lateral cricoarytenoid muscle, or in the paraglottic space prior to the RLN entry into the thyroarytenoid muscle [3].
These studies suggest that the presence of the HCN may be relatively common, though most of these anastomoses occur within the larynx. Outside of cadaveric studies, intraoperative identification of an extralaryngeal HCN has not been described. This is likely related to the tendency of most surgeons to avoid, rather than identify, the EBSLN during thyroidectomy and other central neck surgeries. However, recent literature suggests that routine identification of the EBSLN using loupe magnification and intraoperative neuromonitoring may decrease occult EBSLN injury and improve postoperative voice outcomes [4–6].
The functional significance of the HCN is unclear. It has been suggested that the HCN may be the vestigial nerve of the fifth branchial arch, which has not been identified by anatomists [1, 2]. Some authors have also speculated that the presence of the HCN and other nervous anastomoses within the larynx might explain the variability in position of a paralyzed vocal fold following complete injury or transection of the ipsilateral RLN [1, 2]. In our case, electrostimulation of the HCN produced enough motor activity to elicit a distinct waveform on the neuromonitoring system, suggesting that it contributes to thyroarytenoid muscle function.
The HCN is a connection between the SLN and the RLN that may be relatively common. Functionally, it may contribute to thyroarytenoid motor activity and may in part explain the variability in vocal fold function following injury of the RLN. Intraoperative identification of this variant is rare, since most of the anastomoses occur within the larynx. Newer practice guidelines advocating for the routine identification of the SLN during thyroidectomy may lead to intraoperative identification of more examples of this extralaryngeal variant of the HCN.
FUNDING
This work was supported in part by funds from the Department of Veterans Affairs, BLSR&D and the PNC Foundation (U.D.).
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
The authors thank Ms Trenita Finney for the anatomic illustration. This work was supported in part by funds from the Department of Veterans Affairs BLSR&D, Eye & Ear Foundation and the PNC Foundation (U.D.). This manuscript does not reflect the views of the US Government or the Department of Veterans Affairs. Review of this case was approved by the Institutional Review Board at the University of Pittsburgh.



