-
PDF
- Split View
-
Views
-
Cite
Cite
Meron F. Tesfom, Carole Caldwell, Raveesh Hanasoge, Simon R. Bramhall, Lungs and subcutaneous metastases from a solitary fibrous tumour of the pancreas, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv145, https://doi.org/10.1093/jscr/rjv145
Close - Share Icon Share
Abstract
Solitary fibrous tumour is an uncommon mesenchymal neoplasm previously thought to only originate from the pleura; it is seen only rarely in an extra-pleural location. We report the first case of pancreatic solitary fibrous tumour in an 87-year-old woman that has metastasized to the lungs and subcutaneous tissue. We have identified a solitary mass excised from the groin region, which is positive for CD34 and vimentic marker with high proliferative rate, nuclear atypia and cellular necrosis. Imaging studies confirmed a slow-growing solitary mass in the uncinate lobe of the pancreas with evidence of lung metastasis.
INTRODUCTION
Solitary fibrous tumour (SFT) is an uncommon mesenchymal neoplasm previously thought to only originate from the pleura [1]. Extra-pleura presentations of SFT are rare and generally exhibit benign behaviour. SFTs can be identified using immunohistochemical staining, CD 34 and vimentin are consistently expressed in all pleura and extra-pleural SFTs [2]. Malignant forms of SFT have been described with histological finding of atypia, cellular necrosis, increased mitotic activity and infiltrative margins [2–4]. Pancreatic presentation of SFT is very rare, and to the best of our knowledge, there are no literature reporting metastatic SFT arising from the pancreas.
CASE REPORT
An 87-year-old woman presented to her general practitioner with 2 weeks history of a painless lump in her right groin and was referred to the County Hospital, Hereford. Abdominal examination confirmed a smooth mobile lump 3–4 cm over the right inguinal region, which not a hernia. There were no palpable surrounding lymph nodes. Biochemical and haematological tests, including full blood count, renal and liver function, were all unremarkable.
Her past medical history included hypertension and glaucoma. She has had an episode of acute pancreatitis in January 2007, which was treated with removal of a common bile duct stone, and later she had undergone cholecystectomy for gallstones. The procedures were uneventful. In December 2007, she had recurrent abdominal pain with normal serum amylase level. A computed tomography (CT) scan done in the beginning of 2008 confirmed a 4-cm mass in the uncinate lobe of the pancreas. She was referred to the Regional HPB centre for discussion in their MDT meeting, and an endoscopic ultrasound (EUS) was carried out, which suggested a serous cyst adenoma. As there was no mucin found in the aspirates and the amylase levels were low, a CT scan was done 7 months later. And, this showed the lesion had changed somewhat, but it was believed that this could be due to the EUS aspiration. The Regional HPB MDT recommended an ultrasound scan after 12 months. The ultrasound scan carried out reported the pancreas was poorly visualized due to overlying bowel gas, and a decision was made that the lesion was benign and no further imaging was arranged.
In January 2015, the groin lump was excised intact from the right inguinal region. It measured 55 mm × 42 mm and on microscopy, the mass was found to be a well-demarcated mesenchymal neoplasm, composed of interlacing fascicles of spindle cells with mild/moderate nuclear atypia (Fig. 1a–c). immunohistochemistry showed strong expression of vimentin, CD34 and focal expression of CD10 (Fig. 1d and e). In contrast, SMA, Desmin, MNF116, EMA, S100, HMB45, DOG-1, CD45, AE1/AE3 and CD117 were all negative. INI-1 was retained, and the proliferation index was up to 30% focally. Overall, the histological appearances, immuno-profile and molecular studies have confirmed the diagnosis of a solitary fibrous tumour. In view of the high mitotic activity, the presence of focal necrosis and atypia, this has been regarded as a metastatic malignant solitary fibrous tumour deposit.
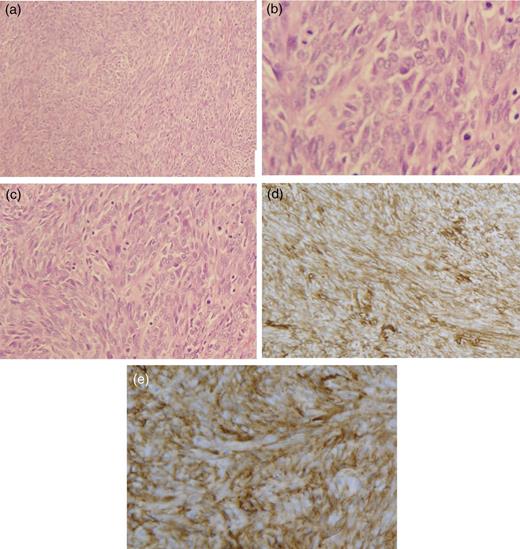
(a–c) Photomicrograph of histologic material shows spindle cells (haematoxylin and eosin staining, ×100 × 200 × 400, respectively). (d and e) CD34 immunohistochemical stain of the resected mass from the groin with tumour cells that have strong positivity.
Following the histological findings, a CT of her thorax, abdomen and pelvis was arranged (Fig. 2). The CT scan reported a large solid cystic mass in the uncinate process of the pancreas measuring 7.2 cm × 4.8 cm in the axial dimension and 7.2 cm in the coronal dimension (Fig. 3). There was displacement of the superior mesenteric vein and artery but no vascular invasion. The CT scan also confirmed lung lesions consistent with metastatic disease (Fig. 3b and c).
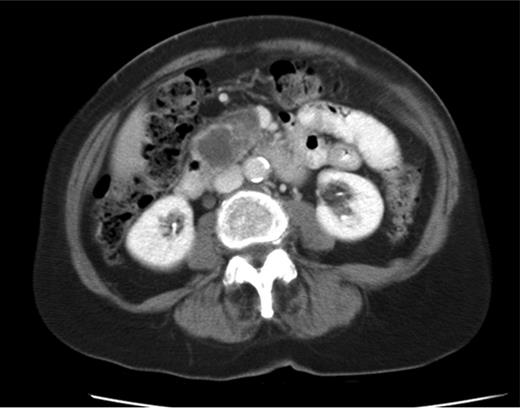
CT shows cystic mass in the uncinate process of pancreas measuring 4 cm in 2008.
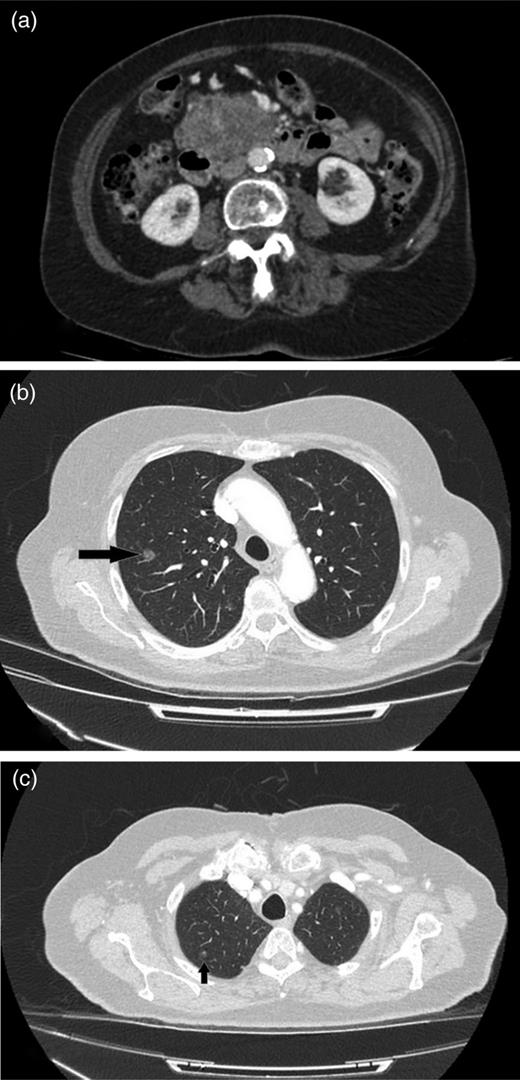
(a) CT image of 2015, a mass lesion in the head of the pancreas with solid and cystic components (bunch of grapes appearance). The lesion measures 7.2 × 4.8 cm in the axial dimension and 7.2 cm in the coronal dimension. (b and c) Multiple focal ground-glass density nodules in both upper lobes of the lungs, largest measuring 1 cm in the right upper lobe.
DISCUSSION
SFT was first described as a spindle neoplasm arising from pleura [1]. However, since then the tumour has been found in extra-pleural sites. SFT is a type of mesenchymal neoplasm of fibroblastic origin. Positive immunohistochemical markers of CD34 and vimentin have been used to identify SFT; other stains like beta-catenin (nuclear) and bcl-2 have also been used in some cases [1, 2, 4].
So far, all previous case reports have identified benign pancreatic SFT with no evidence of metastatic disease [5]. However, SFTs have the potential to metastasize, and a study has shown a metastasis rate of 5.3–5.4% with up to 10% recurrence rate [6]. There has also been two case reports one from central nervous system and kidney SFT which have metastasized to the pancreas [7, 8].
Histologically malignant SFTs have markedly increased cellularity, mitotic activity, nuclear pleomorphism and areas of necrosis [2]. In our case, we have identified a solitary mass excised from the groin region, which is positive for CD34 and vimentic marker with high proliferative rate (30%), nuclear atypia and cellular necrosis. Mesenchymal tumours are generally asymptomatic and slow-growing tumours. Hence, the inguinal mass that developed over 2 weeks is most unlikely to be the primary. The pancreatic mass that appeared as a well-defined mass with cystic portions on radiological images in 2008 measured 4 cm. Over 7 years, the mass increased in size to 7 cm with evidence of metastasis to the lungs. This slow but significant increase in size suggests that the pancreas lesion is the primary. Further investigation such as CT-guided fine-needle aspiration of the pancreatic mass could help to reinforce our findings.
In summary, we here report the first case of primary SFT of the pancreas that has metastasized to the lungs and subcutaneous tissue. Unfortunately, given the patient's age, the potential for lung metastases and the involvement of the vascular structures surgical intervention are not in the best interest of our patient.
CONFLICT OF INTEREST STATEMENT
None declared.



