-
PDF
- Split View
-
Views
-
Cite
Cite
Emily S. Reardon, Linda W. Martin, Boerhaave's syndrome presenting as a mid-esophageal perforation associated with a right-sided pleural effusion, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv142, https://doi.org/10.1093/jscr/rjv142
Close - Share Icon Share
Abstract
There are few published case reports of Boerhaave's syndrome presenting as a mid-esophageal perforation associated with a right-sided pleural effusion. We present an unusual case of spontaneous perforation of the mid-esophagus and discuss the surgical management and outcome. Our case underscores the importance of a meticulous diagnostic and therapeutic approach to the management of an often elusive and difficult disease process.
INTRODUCTION
Boerhaave's syndrome is a rare clinical entity associated with significant morbidity and mortality. While classically described as a post-emetic distal esophageal rupture just proximal to the gastroesophageal junction, presenting with chest pain, pneumomediastinum and a left-sided pleural effusion, the actual presentation is oftentimes nonspecific, mimicking many other clinical disorders and resulting in a delay in diagnosis and therapeutic intervention. Case reports of Boerhaave's syndrome presenting as mid-esophageal perforation associated with a right-sided pleural effusion are particularly uncommon [1–7]. Herein, we present an unusual case and discuss the surgical management and outcome.
CASE REPORT
An 86-year-old female presented to the emergency department with complaints of chest pain and dyspnea after gagging while swallowing a pill. She described the pain as sharp in nature, radiating to her neck, back and epigastrium. Her symptoms were further exacerbated with sips of water. On physical exam, vital signs were normal. She was noted to be anxious; breath sounds were present bilaterally but diminished at the bases, and she had tenderness in the upper abdomen. Chest x-ray demonstrated pneumomediastinum and a right-sided pleural effusion. She was intubated for persistent respiratory distress and transferred to our hospital for further care.
On arrival, she was hemodynamically normal. Pertinent laboratory markers included a white blood cell count of 11, serum bicarbonate of 20 and a lactate of 1.5. A computed tomography (CT) scan of the chest with oral contrast, administered immediately before the study, demonstrated extravasation from the middle third of the esophagus into the right chest and mediastinum with minimal flow distally into the lower esophagus and stomach (Fig. 1). The clinical picture was suggestive of a distal esophageal obstruction from either stricture or neoplasm. Bilateral chest tubes were placed and supportive care initiated, including broad-spectrum antibiotics and fluconazole. An urgent esophagogastroduodenoscopy (EGD) was performed to evaluate for mass or stricture in the distal esophagus, and this showed an obvious perforation with extrusion of fluid and gastric contents noted along the right mid-esophagus with no evidence of stricture or tumor (Fig. 2). The patient was taken to the operating room, and a right posterolateral thoracotomy was performed. Upon entering the chest, murky purulent fluid was noted throughout the right pleural space and mediastinum. Further exploration revealed a transmural perforation in the mid-esophagus, originating at the level of the azygos vein, extending ∼5 cm distally. The right pleural space was debrided and irrigated, and the esophageal tear was repaired primarily after it had been fully exposed. 3-0 Vicryl sutures were placed in an interrupted fashion through the mucosa for the full length of the repair, and this was reinforced with an intercostal muscle flap as the muscular layer of the esophagus was not suitable for repair sutures.
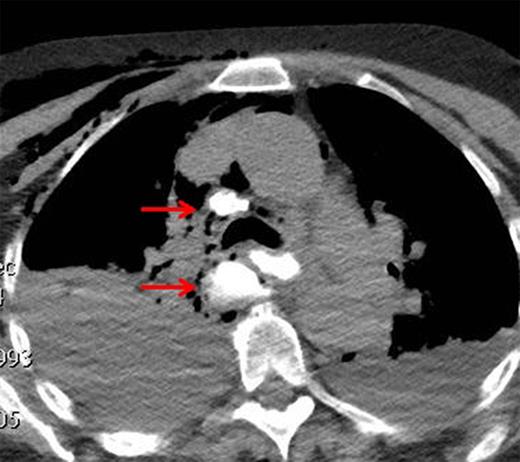
CT demonstrating extravasation of oral contrast into the right chest and mediastinum.
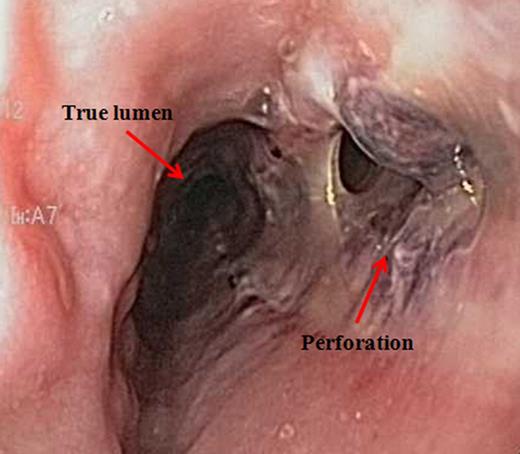
Esophagogastroduodenoscopy confirming site of perforation along the right lateral wall of the mid-esophagus.
She was returned to the intensive care unit and recovered well. An esophagram obtained on Postoperative Day 9 demonstrated no sign of esophageal leak, and she was then started on an oral liquid diet that was advanced to soft foods. Her postoperative course was otherwise uncomplicated. She was discharged on Postoperative Day 17. At follow-up approximately 1 month after surgery, she remained in good health.
DISCUSSION
There are several distinct features about this case worth noting. First, imperative to our patient's good outcome was that the connection between a right-sided pleural effusion and an associated esophageal pathology was immediately recognized. Many of the previously published case reports of Boerhaave's syndrome presenting as a right-sided pleural effusion focus on a delay in diagnosis as a significant contributing factor to persistently high mortality rates [1–5]. Indeed, mortality rates >56% after 24 h and 75–89% after 48 h have been reported [8–10]. In an effort to identify a single salient feature that might clinch the diagnosis, an upright chest x-ray was consistently listed as the most important initial test [1, 2, 4, 5]. It is clear, however, that simply obtaining the appropriate diagnostic tool is not enough. In this case, suspicion for esophageal perforation, in conjunction with the history and radiographic findings, resulted in a quick transfer to our hospital center, where definitive surgical management took place in <24 h.
When presented with a perforation of the mid-esophagus, it is important to evaluate for intrinsic disease of the esophagus, as this will impact both clinical presentation and surgical intervention [8]. Distal obstruction from an esophageal tumor would require esophagogastrectomy, whereas perforation of an otherwise healthy esophagus would be amendable to primary or reinforced repair. This was quickly realized in our case, yet it still remains unclear why our patient's site of rupture was unusual. Other possible causes could have included a peptic stricture, a paraesophageal hernia with obstruction or an underlying dysmotility; none of which were appreciated during our patient's endoscopic exam. The majority of previously reported cases were post-emetic ruptures associated with gastroesophageal reflux and Barrett's esophagus lesions; one was associated with a bleeding duodenal ulcer and another with a hiatal hernia [1–5]. None of these findings, however, would intuitively explain a mid-esophageal perforation.
Our case extends the reported description of Boerhaave's syndrome. It also underscores the importance of a meticulous diagnostic and therapeutic approach to the management of an often elusive and difficult disease process.
CONFLICT OF INTEREST STATEMENT
None declared.



