-
PDF
- Split View
-
Views
-
Cite
Cite
Stina Öberg, Kristoffer Andresen, Jakob M. Møller, Jacob Rosenberg, MRI is unable to illustrate the absorption time of the absorbable TIGR mesh in humans: a case report, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv146, https://doi.org/10.1093/jscr/rjv146
Close - Share Icon Share
Abstract
A male patient had a bilateral laparoscopic inguinal hernia repair in 2012. The right-sided hernia was treated with a permanent mesh, and the left-sided hernia received an absorbable mesh. The absorbable TIGR mesh has been proved to be completely absorbed and replaced by new connective tissue after 3 years in sheep. The patient was therefore followed for 3 years by annual magnetic resonance imagings (MRIs) to illustrate the absorption time in humans. During follow-up, the thickness of the absorbable mesh slightly decreased, and at the last clinical examination, the patient was without a recurrence. However, MRI failed to illustrate absorption of the TIGR mesh, perhaps since new connective tissue and the mesh material had the same appearance on the images. In conclusion, MRI was unable to confirm an absorption time of 3 years for the TIGR mesh, and further studies are needed to investigate if the mesh also completely absorbs in humans.
INTRODUCTION
Inguinal hernias are common, resulting in >20 million inguinal hernia operations performed annually worldwide [1]. The recurrence rate for inguinal hernias declined after the introduction of mesh techniques [2], but an optimal surgical technique to also decrease chronic pain is warranted. Surgeons mostly use permanent meshes, and in recent years, the trend has been to use meshes with less material, which has proved to give less chronic pain [3]. Another type of mesh is the absorbable mesh, which is unique since the material completely absorbs over time. The connective tissue replacing the mesh [4] is thought to prevent recurrences, and the absence of foreign material may decrease the incidence of chronic pain. In fact, one randomized controlled trial that compared a mesh that was absorbed after 6 months with a permanent mesh showed that the absorbable mesh group had significantly less pain after 3 years without any recurrences [5].
The patient in this study had an inguinal hernia operation with the absorbable TIGR mesh, which has been proved to be fully replaced by connective tissue in sheep after 3 years [6]. The patient was therefore followed for 3 years by magnetic resonance imaging (MRI), and the purpose of the study was to illustrate the absorption of the mesh, for the first time in a human. Secondary outcomes were to document any complications throughout the follow-up.
CASE REPORT
An 83-year-old male patient had a bilateral laparoscopic transabdominal pre-peritoneal (TAPP) inguinal hernia repair in the start of 2012. At the preoperative clinical examination, both hernias were palpable and reducible. The surgeon used an absorbable mesh (TIGR Matrix, Novus Scientific) [6] for the left medial hernia and a permanent mesh (Prolene Polypropylene Mesh, Ethicon) for the right lateral hernia. Clinical examinations, imaging and other relevant details during the study period are illustrated as a timeline in Fig. 1.
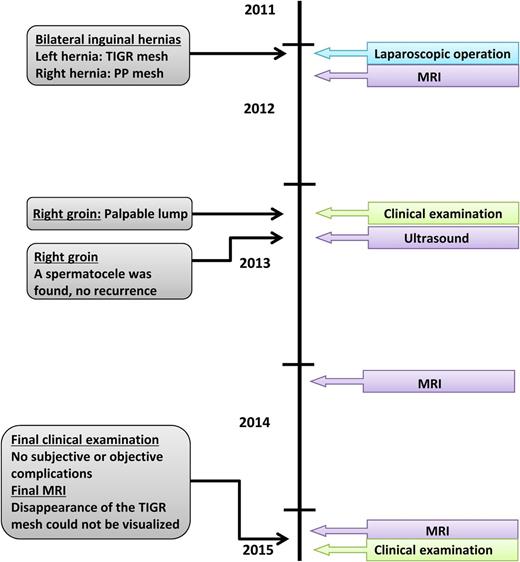
During the follow-up period of 3 years, the patient had three abdominal MRIs (Fig. 2A–D). Both meshes are visible 1 month postoperatively as a dark linear structure (Fig. 2A). When comparing the absorbable mesh 1 month after operation with 2 years after operation (Fig. 2B), the thickness of the dark line had been slightly reduced. The thickness seemed to be unaltered between the second and the third postoperative years (Fig. 2C). The signal voids in Fig. 2B and C have the same intensity, and it is impossible to assess if the dark line seen in the left groin after 2 and 3 years represents the absorbable mesh or new connective tissue. In contrast to this, the thickness of the permanent mesh was stable during the 3 years. The permanent mesh and the absorbable mesh/new connective tissue are also visible in a sagittal image 3 years postoperatively (Fig. 2D).
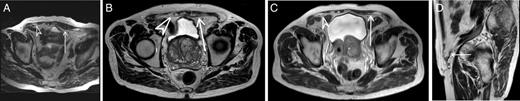
MRIs of the patients’ groins during the follow-up. Arrow indicates the absorbable mesh/new connective tissue. Arrowhead indicates the permanent mesh. Asterisk indicates the permanent mesh. (A) Axial T2-weighted image, 1 month postoperative. (B) Axial T2-weighted image, 2 years postoperative. (C) Axial T2-weighted image, 3 years postoperative. (D) Sagittal T2-weighted image, 3 years postoperative.
One year after the operation, the patient had a clinical examination due to tenderness in the right groin and sensation of a lump, which was diagnosed as a spermatocele by ultrasound and treated conservatively. At the final 3-year clinical examination, the patient had no pain or discomfort and no signs of a recurrence.
DISCUSSION
The MRIs could not confirm full absorption of the TIGR mesh since the mesh and the new connective tissue had the same appearance on the images. At the last 3-year clinical examination, the patient was free of pain, discomfort and recurrences.
Polypropylene meshes are only indirectly visible by MRI [7], and the hypointense dark linear structure visible on the images was either signal void from mesh material or connective tissue. The absorbable TIGR mesh was visible as a dark linear structure 1 month postoperatively. The line was slightly reduced during the first 2 years, but after 3 years, it was impossible to distinguish the absorbable mesh from the new connective tissue formation. The only study investigating absorption time for the TIGR mesh is on sheep, where the authors histologically proved that the mesh was fully replaced by connective tissue after 3 years [6]. Sheep and humans have different metabolism, and therefore, we cannot know if the absorption time will be the same, or if the mesh completely absorbs in humans. To definitely confirm absorption time of the TIGR mesh in humans, it would supposedly be necessary to obtain tissue samples for histological assessments.
A noninvasive way to retrieve information about absorption of the mesh may be to use positron emission tomography (PET). One study has shown visualization of permanent meshes by PET, due to a foreign body reaction around the meshes, 3–10 years after the initial inguinal hernia operation [8]. Inflammatory processes have also been visible by PET in other studies [9, 10], and since the animal study on the TIGR mesh showed a chronic inflammation lasting for 3 years [6], TIGR meshes may be visualized by PET during the absorption period. It is unknown if the foreign body reaction ends directly after the mesh has been absorbed, but if we presume that this is the case, PET may be an option to confirm the absorption time.
The strengths of this study were that the patient had MRIs of the groins during the 3-year follow-up period, which was anticipated to be enough time for the absorbable mesh to be completely absorbed [6]. The limitation of this study was that the meshes could not be directly visualized, which made it impossible to illustrate full absorption of the mesh and validate the findings of the MRIs. At the end of the study, the patient had no chronic pain and had not developed a recurrence. Since we are unsure if the mesh was fully absorbed after 3 years, we do not know if the connective tissue by itself has the ability to prevent a recurrence in all patients.
In conclusion, the absorbable TIGR mesh and new connective tissue had the same appearance on MRI, and we were therefore unable to confirm that the absorption time of 3 years seen among sheep also was true for humans. Further studies are needed to confirm the absorption time of the TIGR mesh in humans.
CONFLICT OF INTEREST STATEMENT
K.A. reports personal fees from Bard outside the submitted work. J.R. reports grants from Johnson & Johnson, grants and personal fees from Bard, personal fees from Merck, outside the submitted work.



