-
PDF
- Split View
-
Views
-
Cite
Cite
Martin A. Benjamin, Garrett Schwarzman, Mariet Eivazi, Lawrence Zachary, Autologous staged fat tissue transfer in post-traumatic lower extremity reconstruction, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv141, https://doi.org/10.1093/jscr/rjv141
Close - Share Icon Share
Abstract
Autologous fat tissue transfer for aesthetic reconstruction has been described in the literature for soft tissue damage as early as 1893. One area that has yet to be described is the role of fat grafting in post-traumatic lower extremity injuries. In this case report, we present a patient who had significant injury to her right lower extremity and presented for reconstruction. The patient is a 52-year-old female who presented to clinic after a right lower extremity traumatic injury that required multiple re-operations, which lead to dense scarring and volume loss along the extremity inferior to the knee joint. The patient received two staged autologous fat injections and reported positive outcomes. Our case report demonstrates the utility of fat transfer in reconstruction of the lower extremity in staged fashion. Further research in the refinement of this technique and patient follow-up will lead to better graft survival and reconstructive outcomes.
INTRODUCTION
Autologous fat transplantation as a means for aesthetic reconstruction has been described in the literature for soft tissue damage as early as 1893. Liposuction, purification and re-implantation are referred to as the primary steps in performing autologous fat grafting [1]. Unfortunately, the ease of harvesting this material for reconstruction was negated by the fact that it had poor reliability and inconsistency in terms of graft survival over time [2, 3].
There is no set of standards or indications for when fat grafting should or should not be used to date. Fat transfer has also been used in hand rejuvenation, contour deformities and, in the case of our patient, lower extremity deformities [2]. Fat transplantation is ideal for deformities because adipocytes are stable, immunologically silent, not allergenic and are often in excess and cheap [1]. The procedure is inherently unpredictable though, especially when attempting to predict the amount of resorption of the fat tissue. Quite often, a series of procedures may be needed to ensure the desired outcome.
Fat grafting is a common procedure for facial rejuvenation and reconstruction but has not been frequently described in the treatment of post-traumatic lower extremity injuries. In this case report, we present a patient who had significant damage to her right lower leg from a motor vehicle accident. Given the history of fat transfer use in repairing soft tissue damage, we attempted to reconstruct the patient's right lower extremity in a staged fat transfer fashion. The outcome of this study lends credence to the viability of autologous fat transfer as a viable option for lower extremity reconstruction post-traumatic event.
CASE REPORT
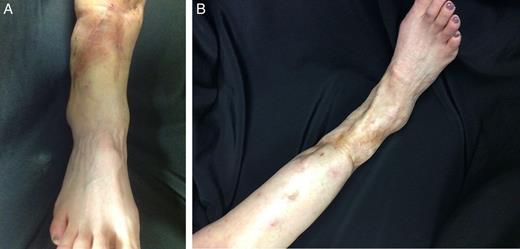
The patient is a 52-year-old female who presented to plastic surgery clinic to discuss functional and cosmetic reconstruction of her right lower extremity. The patient was involved in a traumatic injury requiring fixation of the right leg along with several subsequent skin grafts that led to dense scarring and volume loss along the entire right leg. The patient suffered from neuralgias, stiffness and severe psychosocial stigmata associated with the scar formation (see Fig. 1) and sought definitive reconstruction.

The patient underwent the initial autologous staged fat transfer procedure on 9 April 2012. Approximately 500 cc of fat was harvested from the abdomen, knees, hips and flanks. This fat was then processed into several tuberculin syringes and prepared for injection. Prior to injection, the patient underwent circumferential release of the 8 cm extremity scar via excision and sharp dissection through use of sharp-tipped steel dissection scissors. The processed fat was injected into multiple areas of the scar subcutaneously in 2 cc injections at a time. A total of 57 cc of fat was injected in the lower extremity during this procedure and elevated the scar tissue from the bone.
The patient underwent the second stage of release of scar and fat transfer in 17 August 2012. Approximately 80–90% of the fat transfer from the previous injection had incorporated into the right lower extremity. The second stage began in similar fashion with liposuction and processing of fat obtained from knees, hips and flanks via loop lavage. The port sites were closed with fast-absorbing catgut suture and Steri-strips. After removing ∼700 cc via Coleman catheter, the patient had the fat instilled into her right lower extremity in 1–2 cc aliquots. Approximately 144 cc of fat was instilled into areas of tendon exposure superficially to release the contracture of the scar from her previous operations. The patient had dry sterile non-woven gauze dressing, and an elasticated bandage was placed around this extremity for compression and would follow up in 1 week.
The post-operative course was not complicated, and a drastic improvement was noted in both form and appearance of the patient's lower extremity after the staged fat transfer reconstruction procedure (see Fig. 2). The patient noted improvement in mobility and decreased neuralgic pain that she had described prior to the procedure. Most importantly, the patient appreciated the symmetry between her lower extremities and reported improved self-esteem and decreased anxiety regarding her medical condition (see Fig. 3).

DISCUSSION
The majority of fat grafting published in the literature pertains to facial injuries and reconstruction with scant publications in reference to lower extremity reconstruction. One notable study conducted in 2008 did analyse a series of patients with autologous fat tissue transfers for lower limb atrophies. In this particular series, 20 patients with either localized or circumferential atrophies of the lower extremities were enrolled for multistage autologous fat tissue transfer. The reasons for the atrophies included traumatic (60%), congenital (25%) and iatrogenic (15%). It was found that at 2-year follow-up the patients had on average a 1.9 cm augmentation, with a range of 1–6 cm, and most were highly satisfied with the outcome [2]. Although the study was not randomized and satisfaction is a subjective criterion, it does show that lower extremity fat grafting is a viable option for tissue growth.
The common complications that arise from staged autologous fat transfer procedures are bleeding and infection. One rare complication discussed was the possibility of graft hypertrophy. The reported case demonstrated that at 10-year follow-up for a fat-grafting patient, the graft had hypertrophied to an extent where it was no longer cosmetically acceptable. It was theorized that the mechanism behind this hypertrophy involved an over-deposition of collagen as similarly seen in keloid formation. The lack of data on the subject, however, limits the predictability of the outcome and is an area that requires further study.
In our patient, the staged fat transfers occurred over a period of 4–5 months and included ancillary rehabilitation between injections. Although the process of autologous fat transfer in the lower extremity is similar to that used in the face, the technique has not often been employed in extremity reconstruction. Although typically thought to be associated with aging, volume loss remains a critical challenge of lower extremity reconstruction post-traumatic event. We suggest that a staged autologous fat transfer has become an important tool for both volume replacement and aesthetic reconstruction of the lower extremity. Further research in the refinement of this technique and long-term patient follow-up will likely lead to even better graft survival and patient reconstructive outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.



