-
PDF
- Split View
-
Views
-
Cite
Cite
Jiten P. Kalyan, Ali Kordzadeh, Muhammad A. Hanif, Mathew Griffiths, Harry Lyall, Ioannis Prionidis, Nonunion of the tibial facture as a consequence of posterior tibial artery pseudoaneurysm, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv138, https://doi.org/10.1093/jscr/rjv138
Close - Share Icon Share
Abstract
Pseudoaneurysm of the posterior tibial artery (PTA) is uncommon, and they mainly occur following high-velocity trauma, open fractures and can be iatrogenic in nature. To the best of our knowledge, this is the first reported and successfully treated case of PTA pseudoaneurysm identified as a consequence of tibia fracture nonunion in an otherwise healthy young individual 6 months following the original incident with a novel intraoperative technique.
INTRODUCTION
Nonunion of a fracture can pose a significant challenge in terms of skeletal stability, soft tissue biomechanics and potential limb loss. They most commonly occur as a consequence of infection, mal-alignment, metabolic and endocrine abnormalities [1]. However, in otherwise healthy young individuals, such etiologies are rare and alternative pathological factors should be considered. Herein, we present the first reported and successfully treated case of tibal fracture nonunion as the result of posterior tibial artery (PTA) pseudoaneurysm.
CASE REPORT
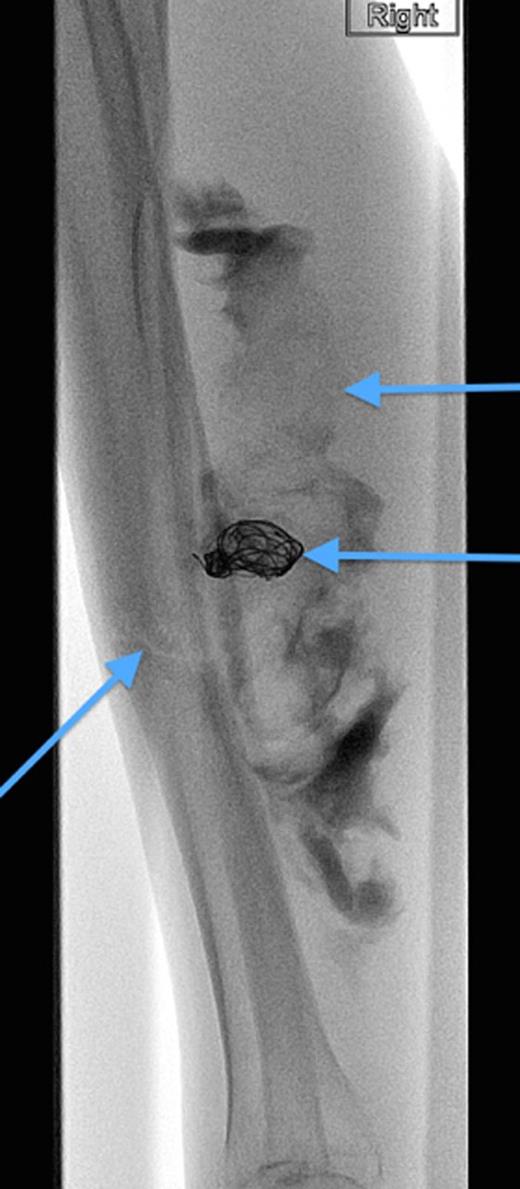
A 20-year-old man with no past medical history presented to the emergency department with non-displaced and closed transverse fracture of the left mid-tibial shaft and an intact fibula induced by a tackle during a football match. On examination, he had no neurovascular deficit and all crural pulses were palpable. His fracture was treated conservatively with a non-weight bearing above knee plaster cast later replaced by a below knee cast for a total period of 6 months. Upon examination during his attendance to the facture clinic, x-ray demonstrated no signs of fracture union. The subsequent magnetic resonance imagining (MRI) confirmed a nonunion of the fracture along with an ovoid 2.7 cm posterior compartment vascularized mass causing bowing of the interosseous septum with no evidence of avascularity of the bony margins (Fig. 1). This was confirmed to be a pseudoaneurysm originating from the PTA. An endovascular approach was adopted, and the pseudoaneurysm was injected with 2 ml of thrombin, filled with multiple coils and deployment of an angiography balloon (in the sac) (4 mm × 6 cm) for 7 min (Fig. 2). This resulted in complete cessation of the pseudoaneurysm with normal flow in the PTA (Fig. 3). The residual extravasated hematoma was later drained by an open approach. Follow-up x-ray (6 months) demonstrated complete union of the fracture site with no associated complications.

MRI images demonstrating the site, size and the origin of the PTA pseudoaneurysm.
Angiographic image, demonstrating the site of the nonunion, coil insertion to the pseudoaneurysm and extravasated contrast.
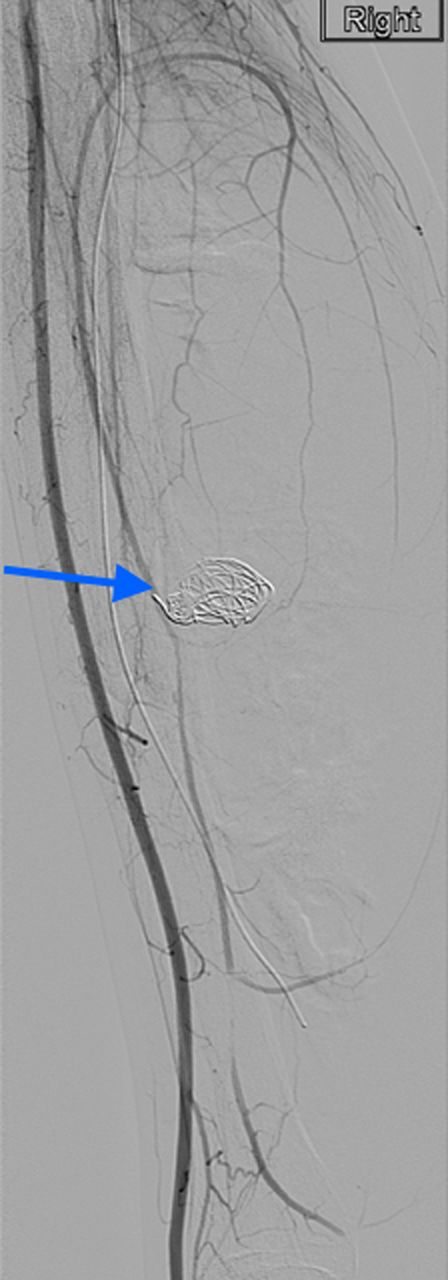
Complete resolution of the pseudoaneurysm and confirmed patent PTA.
DISCUSSION
Pseudoaneurysms of the PTA are rare, and they mainly occur following sudden acceleration and/or deceleration type injury, open fractures and, in few cases, can be iatrogenic (manipulation of fracture, surgery and Ilizarov K-wire) [2, 3]. Currently, no report in the literature suggests a single isolated and close fracture of tibial bone to be responsible for pseudoaneurysms of PTA.
They are mainly asymptomatic and present as a pulsatile lump but in their deeper anatomical course could result in tibial nerve compression causing paresthesia, neuralgia and weakness of the foot and toe muscles [4]. In 3–9% of reported series, they present with signs and symptoms of lower limb ischemia following pseudoaneurysms thrombosis and/or distal embolization [4, 5]. Rarely, they rupture and cause compartment syndrome [6]. In our reported case, the patient did not exhibit any neurovascular deficit, and it was an incidental finding following investigations for the tibial fracture nonunion. Furthermore, fracture nonunion in a healthy young individual without any risk factor is rare and should raise suspicions about alternative and infrequent pathologies.
The management of pseudoaneurysms of PTA is varied, and they depend on the individual's symptomatology and the subsequent course of the pseudoaneurysm. Currently, there is no consensus on their overall management; therefore, indications for their open versus endovascular repair are subjected to various debates [7]. Any repair should aim at their complete exclusion and/or excision from the main vessel. Open repair (ligation and/or excision and interposition vein grafting) in deep anatomical areas may subject the patient to extensive dissection, longer operative time and higher incidences of morbidity (motor and sensory nerve damage, prolonged recovery, deep vein thrombosis) [8]. Endovascular repair is another acceptable option, but this approach has its own limitations. The deployment of any type stent for exclusion of pseudoaneurysm from the main artery in the infra popliteal region is known to possess low patency and thrombotic incidences. The use of thrombin, coils and glue remains another alternative, but this mainly depends on the pseudoaneurysm neck size, as wider necks fail to contain the above and can result in failure of the procedure and thrombosis of the remaining artery [9]. Overall, the approach should be tailored according to the patient's arterial status and features of the pseudoaneurysm. To the best of our knowledge, deployment of angiography balloon (as an occlusive technique) in addition to thrombin and coil for the exclusion of PTA pseudoaneurysm has not been reported in the literature. The use of this novel technique could be beneficial in exclusion of wider neck pseudoaneurysms and limitations of the damage to the main vessel as reported in the current case report.
In the reported case, the individual did not exhibit any signs and symptoms of pseudoaneurysms and similarly did not raise any suspicion of such pathology till nonunion was detected. Once suspected, the best investigative modality is computed tomography angiography (CTA) followed by magnetic resonance imaging (MRI). Both of these modalities have sensitivity and specificity of more than 90% for detection of isolated entities [10].
In conclusion, nonunion of fractures in young healthy individuals should raise the suspicion of pseudoaneurysms, despite the absence of clinical signs and symptoms of vascular disruptions. Clinicians should have low threshold for CTA and/or MRI in such circumstances, and the surgical method of repair (open versus endovascular) should be in accordance with the patient's best interest.
Written informed consent was obtained from the patient for publication of this case report and accompanying images. No identification details have been used.
CONFLICT OF INTEREST STATEMENT
None declared.



