-
PDF
- Split View
-
Views
-
Cite
Cite
Arjun S. Chandran, Stephen Honeybul, A case of psychosis induced self-insertion of intracranial hypodermic needles causing seizures, Journal of Surgical Case Reports, Volume 2015, Issue 1, January 2015, rju145, https://doi.org/10.1093/jscr/rju145
Close - Share Icon Share
Abstract
Self-insertion of foreign bodies is a rare event. This report details a 56-year-old male who had self-inserted six hypodermic needles into his left frontal lobe 6 years previously. He subsequently presented with seizures and went on to have the needles surgically removed. This represents the first case of its type involving hypodermic needles. Given that intracranial needles are a rare finding, the management of such patients is complex. Two management issues in particular that require consideration are: (i) can the needles be left in situ and (ii) does removal of the needles reduce the risk of seizures in the long term?
INTRODUCTION
The self-insertion of foreign bodies is a rare event, insertion into the intracranial cavity even more so. This report details the first known case of intracranial hypodermic needles. The rarity of such a finding makes management of such patients complex. Conservative management, leaving the needles in situ, is an option but can lead to adverse neurological sequelae and seizures. Whether this risk potentiates the need to expose the patient to operative complications is debatable. We present the first reported case of intracranial hypodermic needles and explore the available literature on intracranial needles and potential management strategies.
CASE REPORT
A 56-year-old male was transferred from a local hospital following a generalized tonic–clonic seizure. Computed tomography (CT) of the brain confirmed the presence of six intracranial needles that appeared to have been inserted into the left frontal lobe through the frontal sinus.
The patient has a background history of schizophrenia, and amphetamine and marijuana abuse. The patient described a psychotic episode 6 years ago that had occurred following several days of amphetamine use. This episode culminated in him acquiring a number of clean, unused hypodermic needles from a local pharmacy. He then proceeded to insert them through the glabella region and into his brain. The patient clearly remembered and reported that this was not an attempt at suicide. He described using a folded magazine to remove the ends of the needle, leaving them flush with the skin, and he suffered no neurological sequelae as a consequence of these actions. At the time he told no one about these events, sought no medical help and shortly thereafter he ceased all recreational drug usage.
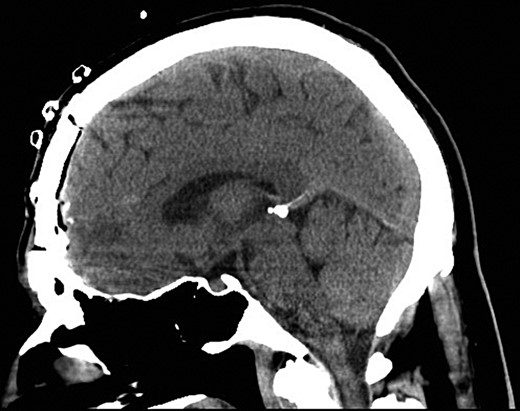
Following the current presentation, he was commenced on levetiracetam and a CT angiogram was performed to rule out an intracranial vascular injury. A preoperative CT slice and three-dimensional (3D) reconstruction of the needles in-situ is provided in Figs 1 and 2.

Preoperative sagittal CT demonstrating six needles traversing through the frontal lobe.
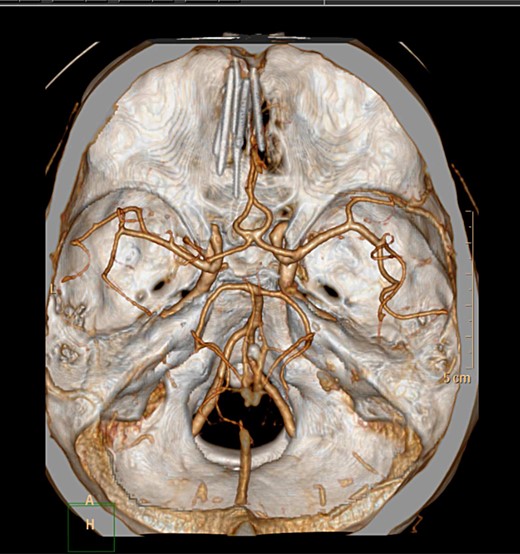
Axial CT 3D reconstruction showing six needles traversing intracranially and their relationship to vascular structures.
The patient had a bi-frontal craniotomy to remove the needles. As the bone flap was elevated, one needle, which was attached to the bone, was removed. The remaining five needles were seen penetrating through the dura. These were pulled out through the dura with ease. No dissection of the needles was required. Durotomy was performed to assess the frontal lobe surface. Puncture marks in the cortical surface were evident; however, no significant hemorrhage or gross pathological abnormalities were noted.
The patient had three postoperative seizures within 24 h of the surgery. He was commenced on phenytoin in addition to levetiracetam. The postoperative period was otherwise unremarkable. A postoperative CT was performed which demonstrated removal of all needles (Fig. 3). He was discharged home Day 3 with no further seizures. The patient remained seizure free at 6-month follow-up.
Sagittal postoperative CT scan demonstrating successful removal of the needles.
DISCUSSION
The insertion of a foreign body into the intracranial compartment most commonly occurs as a result of high velocity injuries involving firearms and other trigger operated devices such as spear and nail guns [1]. A less common but well documented intracranial foreign body finding is that of sewing needles that have been inserted through the anterior fontanelle in what is believed to be a failed attempt at infanticide [2–4].
The deliberate self-insertion of a foreign body intracranially is far less common; although this can occur as a result of attempted suicide, this is by no means always the case. A diagnosis of a psychotic illness has been reported in ∼50% of cases and it is unusual for the outcome to fatal, presumably due to the low energy involved (when compared with a gunshot injury) [1].
The current case is unusual in that it represents the only reported case of self-inflicted intracranial insertion of hypodermic needles and a number of management issues require consideration.
If the foreign bodies are discovered incidentally, consideration can be given to conservative management. Although there is limited evidence from the literature, that which is available comes mainly from reports of intracranial sewing needles.
Leaving the needles in situ poses a number of risks, including potential future seizures [4–6], headaches [7], infection [8] and migration of the needles and subsequent neurological injury [9]. However, surgery exposes an individual to operative complications.
Epileptogenesis of the intracranial needles appears to be related to the development of rust [5]. One theory is that the rusting process turns one end of the needle into a cathode and the other an anode, creating a pseudo-galvanic cell. Removal of the needle should, at least theoretically, remove most of the epileptogenic stimulus. While removal of intracranial sewing needles has been reported as leading to cessation of seizures in the short term [5, 10], it may be best to adopt a relatively guarded prognosis in terms of long-term seizure control.
An alternative approach would be to manage seizures with anticonvulsant therapy in cases where surgical removal is either declined or thought to be hazardous, and this approach has also been reported to be successful [6].
This is a relatively unique case that presented a number of interesting management issues. The main aim of removing the needles was to reduce the risk of infection and reduce the risk of ongoing seizures. While this appears to have been successful, long-term follow-up will be required to establish that this has occurred.
CONFLICT OF INTEREST STATEMENT
None declared.



